When a drug has a narrow therapeutic index, even tiny changes in how much of it enters your bloodstream can mean the difference between effective treatment and dangerous side effects. This isn’t theoretical - it’s life-or-death for people taking drugs like warfarin, digoxin, or levothyroxine. That’s why regulators have put in place much stricter rules for generic versions of these medications. These aren’t just minor tweaks. They’re major shifts in how bioequivalence is measured, tested, and approved - all to keep patients safe.
What Makes a Drug Have a Narrow Therapeutic Index?
A drug is classified as having a narrow therapeutic index (NTI) when the gap between a safe, effective dose and a toxic one is very small. The FDA defines this as a therapeutic index of 3 or less. That means if the dose goes up just 33%, you could hit a dangerous level. For comparison, most medications have a therapeutic index of 10 or higher - meaning you’d need to take three to ten times the normal dose before toxicity becomes a concern. Common NTI drugs include:- Warfarin (blood thinner)
- Levothyroxine (thyroid hormone)
- Digoxin (heart medication)
- Phenytoin (anti-seizure drug)
- Tacrolimus (immunosuppressant for transplant patients)
- Lithium carbonate (mood stabilizer)
Why Standard Bioequivalence Rules Aren’t Enough
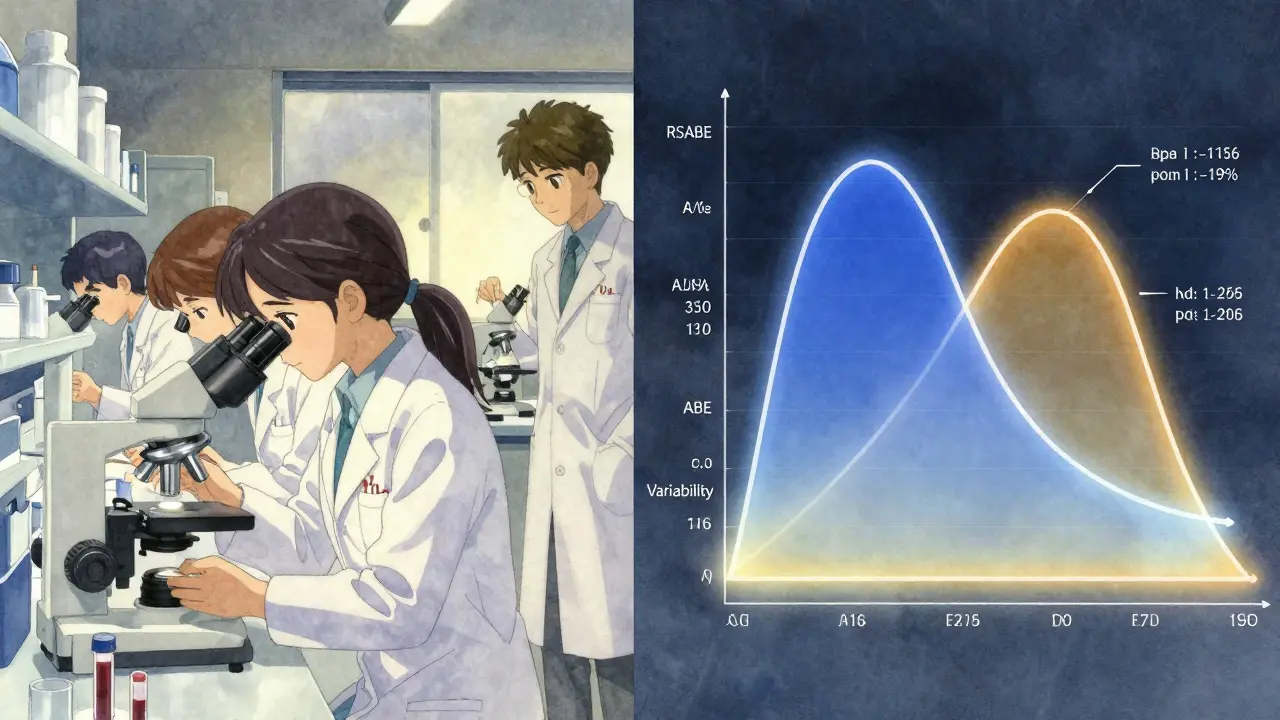
For most generic drugs, regulators accept bioequivalence if the generic’s absorption matches the brand-name drug within 80% to 125%. That’s the standard range for average bioequivalence (ABE). It works fine for drugs where small differences in blood levels don’t cause harm. But for NTI drugs, that 80-125% window is too wide. A 20% drop in blood concentration of warfarin could mean a clot forms. A 20% spike could cause dangerous bleeding. That’s why regulators had to rethink the rules. The FDA’s 2015 guidance on NTI drugs was the first major step. It didn’t just tighten the numbers - it changed the entire testing model. Instead of just comparing average blood levels, they now require three separate tests to prove safety.The FDA’s Three-Part Bioequivalence Test
The FDA’s current approach for NTI drugs is the most detailed in the world. To get approval, a generic version must pass all three of these criteria:- Reference-Scaled Average Bioequivalence (RSABE): This adjusts the acceptable range based on how variable the original drug is in patients. If the brand drug’s levels bounce around a lot, the generic is allowed more wiggle room - but only if it’s just as variable. If the generic is more variable, it fails.
- Variability Comparison: The generic must not be more variable than the brand. The upper limit of the 90% confidence interval for the ratio of within-subject standard deviation (test vs. reference) must be ≤ 2.5. This is a statistical test that ensures the generic behaves as consistently as the original.
- Unscaled Average Bioequivalence (ABE): Even after passing RSABE and variability, the generic must still fall within the traditional 80-125% range for both AUC and Cmax. This acts as a final safety net.
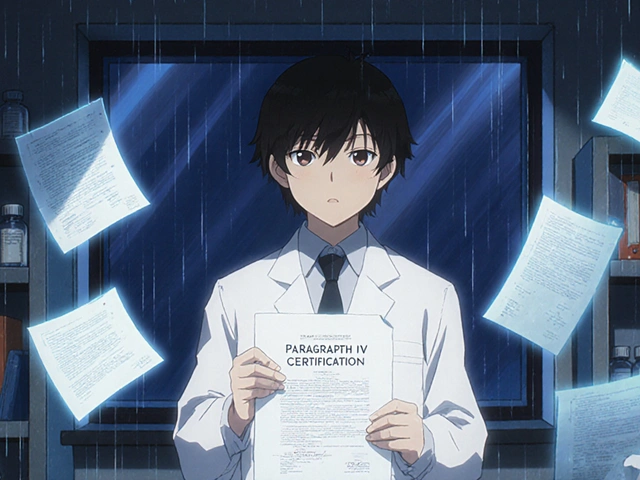
How Other Regulators Compare
The FDA isn’t alone in tightening rules, but its method is unique. The European Medicines Agency (EMA) uses a fixed, narrower range: 90-111% for both AUC and Cmax. It’s simpler, but less flexible. If a drug has low variability, the EMA still applies the same 90-111% limit - even if a wider range might be safe. Health Canada uses a slightly different standard: 90.0-112.0% for AUC for critical dose drugs. They don’t require the variability comparison that the FDA does. The FDA’s approach is more scientifically precise because it adapts to the drug’s behavior. But it’s also more expensive. Industry estimates put the cost of an NTI bioequivalence study at $500,000 to $1 million - nearly double the cost of a standard generic study. That’s a major barrier for smaller manufacturers.Real-World Evidence Supports the Stricter Rules
Critics argue that these strict rules might slow down generic competition and raise prices. But real-world data tells a different story. A 2017 study in the American Journal of Transplantation looked at transplant patients switched from brand-name tacrolimus to a generic version. Using the FDA’s NTI criteria, researchers found no difference in rejection rates or side effects. Another study in Circulation: Cardiovascular Quality and Outcomes in 2019 showed no increase in bleeding or clotting events when patients switched from brand to generic warfarin. These aren’t isolated cases. Across multiple NTI drugs, when generics meet the stricter standards, they perform just as safely as the originals.Why Generic Market Share for NTI Drugs Is Still Low
Despite the evidence, generic adoption for NTI drugs lags behind other medications. In 2021, the average generic market share for NTI drugs was only 68%, compared to 90% for non-NTI drugs. Why? Two big reasons:- Prescriber hesitation: Many doctors still prefer brand-name drugs for NTI medications, fearing small differences might hurt patients - even though science says otherwise.
- Cost and complexity: The high cost of testing makes it less attractive for generic companies. With a $1 million price tag per study, many companies wait for a few big NTI drugs to be approved before investing.

What’s Next for NTI Drug Regulation?
The big question now is harmonization. Right now, each region has its own rules. A generic drug approved in the U.S. might not meet EMA standards, and vice versa. That forces manufacturers to run multiple studies - increasing costs and delaying access. Experts predict that by 2026, regulators may align more closely on NTI standards. McKinsey & Company estimates that harmonization could cut development costs by 15-20%. That’s a game-changer for generic manufacturers. The FDA is also working on publishing a comprehensive list of NTI drugs. Right now, they don’t maintain one. Instead, they issue product-specific guidance for each drug individually. That creates confusion for companies trying to plan their pipeline.What This Means for Patients
You might not think about bioequivalence standards - but they directly affect your safety and access to affordable medication. If you’re taking levothyroxine or warfarin, you deserve a generic version that’s just as reliable as the brand. The stricter rules exist because we’ve learned, the hard way, that small differences matter. And when they do, the consequences can be severe. The good news? When generics meet these standards, they’re just as safe. The challenge is making sure enough manufacturers are willing to invest in the testing - and that doctors and patients trust the results. More data, better guidelines, and international alignment are coming. But the goal hasn’t changed: protect patients without blocking access to affordable medicine.NTI Drugs and Generic Alternatives: What You Should Know
If you’re on an NTI drug and your pharmacist switches you to a generic, here’s what to do:- Ask if the generic has been approved under the FDA’s NTI bioequivalence criteria.
- Don’t assume all generics are the same - some may not meet the stricter standards.
- Monitor for changes in symptoms. For warfarin, that means checking INR levels more closely after a switch.
- Speak up if you notice anything off. Your doctor may need to adjust your dose.
What does 'narrow therapeutic index' mean for a drug?
A narrow therapeutic index means the difference between a safe, effective dose and a toxic dose is very small. Even small changes in blood levels - like 10-20% - can lead to treatment failure or serious side effects. Drugs like warfarin, digoxin, and levothyroxine fall into this category.
Why are bioequivalence requirements stricter for NTI drugs?
Because small differences in absorption can cause harm. Standard bioequivalence limits (80-125%) are too wide for these drugs. Stricter rules ensure generic versions behave almost identically to the brand-name drug, preventing dangerous fluctuations in blood concentration.
What are the FDA’s bioequivalence requirements for NTI drugs?
The FDA requires three criteria: 1) Reference-scaled average bioequivalence (RSABE), which adjusts limits based on the brand drug’s variability; 2) A variability comparison where the test drug’s variability must not exceed 2.5 times the reference drug’s; and 3) Unscaled average bioequivalence within the 80-125% range. All three must be met.
How do EMA and Health Canada’s rules differ from the FDA’s?
The EMA uses a fixed 90-111% bioequivalence range for NTI drugs. Health Canada uses 90.0-112.0% for AUC. Neither requires the variability comparison or reference-scaling that the FDA does. The FDA’s method is more complex but more tailored to each drug’s behavior.
Are generic NTI drugs safe?
Yes - if they meet the stricter regulatory standards. Real-world studies show no increase in adverse events when patients switch from brand to generic versions of warfarin, tacrolimus, or levothyroxine, as long as the generics passed the FDA’s NTI bioequivalence tests.
Why aren’t more generic NTI drugs on the market?
Because the bioequivalence studies are expensive - often $500,000 to $1 million per drug - and more complex than for regular generics. This discourages manufacturers, especially smaller ones. Plus, some prescribers still prefer brand-name drugs due to lingering concerns, even though evidence supports safety.
Will NTI drug regulations become more consistent worldwide?
Yes. Experts predict international harmonization by 2026, with regulators aligning on testing methods and acceptance criteria. This could reduce development costs by 15-20% and speed up generic access without compromising safety.




Comments
brooke wright
This is wild-I had no idea switching my levothyroxine brand could be this risky. My pharmacist just swapped it out last month and I didn’t think twice. Now I’m sweating bullets checking my bloodwork. 😅
Nick Cole
Look, I get why the FDA’s rules are strict-but the cost is insane. $1M per study? That’s not regulation, that’s a barrier to entry for anyone without a pharma corporate backer. We’re not protecting patients-we’re protecting Big Pharma’s monopoly on NTI generics. And yes, I’ve seen the data. It’s solid. But the system’s rigged.
Nicholas Gabriel
Let’s be clear: the FDA’s three-part test isn’t overkill-it’s science. Seriously. RSABE? Variability comparison? Unscaled ABE? Each one exists because someone, somewhere, had a heart attack-or a stroke-or a transplant rejection-because a generic was ‘close enough.’ And now? We have data that proves it works. So why are we still arguing? We’ve solved the problem. Now we just need to scale it.
And yes, it’s expensive. But the cost of a single adverse event? That’s way higher. And if you’re a small manufacturer? Partner with a university. Apply for FDA expedited pathways. Don’t give up. Patients are counting on you.
Isabella Reid
My mom’s been on warfarin for 12 years. She switched to a generic last year and her INR’s been rock steady. No bleeding, no clots, no drama. The docs still act like it’s a gamble-but the numbers don’t lie. Maybe it’s time we stop treating patients like lab rats and start trusting the science?
Jody Fahrenkrug
Just had my pharmacist switch me to a generic tacrolimus. Asked if it met the NTI standards. She said yes. Didn’t even blink. I’m just glad someone’s doing the work so I don’t have to. 🙏
Kasey Summerer
So let me get this straight… we spend a million bucks to prove a generic isn’t going to kill someone… and then we still get side-eye from doctors? 😂 I mean, congrats, we invented the most expensive placebo test in history. Next up: FDA-approved coffee that won’t give you anxiety. ☕️
Allen Davidson
Look, I get the fear. I do. But the data’s been clear for years. If the generic passes the FDA’s triple-check system, it’s as safe as the brand. The real issue? Trust. And trust doesn’t come from studies-it comes from stories. So if you’re a doc, talk to your patients. If you’re a patient, ask your pharmacist: ‘Did this pass the NTI criteria?’ If they don’t know, they’re not doing their job.
We’re not fighting generics. We’re fighting ignorance. And that’s the only thing that’s truly dangerous.
john Mccoskey
Let’s cut through the regulatory fluff. The FDA’s ‘three-part test’ isn’t innovation-it’s institutional overcompensation. You want to ensure safety? Standardize the dosing. Enforce pharmacy-level batch tracking. Mandate real-time therapeutic drug monitoring for NTI drugs. But no-instead, we invent a bureaucratic labyrinth that only big pharma can navigate, then call it ‘science.’ The real problem isn’t bioequivalence-it’s the pharmaceutical-industrial complex’s addiction to complexity as a profit mechanism. You don’t need three tests. You need transparency. You need traceability. You need accountability. Not another 50-page guidance document written by someone who’s never held a pill in their hand.
And don’t get me started on ‘harmonization.’ That’s just regulatory colonialism dressed up as cooperation. The EMA’s 90-111% range isn’t ‘simpler’-it’s more honest. It doesn’t pretend to be adaptive. It just says: ‘If it’s this dangerous, then don’t f*ck around.’ Why can’t we all just do that?
Stop romanticizing bureaucracy. Stop calling expensive gatekeeping ‘safety.’ Real safety is accessible, affordable, and monitored-not locked behind a $1M audit trail.