How to Make a Medication Action Plan with Your Care Team
Nov 16 2025
When anaphylaxis during chemo, a severe, rapid allergic reaction triggered by chemotherapy drugs. It’s not common, but when it happens, it demands immediate action. Unlike mild side effects like nausea or fatigue, anaphylaxis hits fast—often within minutes of the infusion starting. Symptoms include swelling in the throat, trouble breathing, a sudden drop in blood pressure, hives, and dizziness. If you’ve ever had a bad reaction to a drug before, your risk goes up. But even people with no history of allergies can react unexpectedly.
Some chemotherapy drugs are more likely to cause this than others. pegaspargase, a key drug used in leukemia treatment is one of the biggest culprits. Others include oxaliplatin, commonly used for colorectal cancer, and paclitaxel, used in breast and lung cancer. These drugs don’t just kill cancer cells—they can also trigger your immune system to overreact. The body mistakes them for invaders and releases massive amounts of histamine, causing the crash in blood pressure and airway swelling that defines anaphylaxis.
What makes this even trickier is that some symptoms look like chemo side effects. A rash could be from the drug, or it could be the first sign of anaphylaxis. A spike in heart rate might be stress—or it might be your body going into shock. That’s why hospitals always monitor patients closely during the first 15 to 30 minutes of any chemo infusion. Nurses check your breathing, blood pressure, and skin for any changes. If you feel anything unusual, speak up. Don’t wait. Anaphylaxis can turn deadly in under five minutes.
Prevention starts with your medical team. If you’ve had a reaction before, they’ll likely pre-medicate you with steroids and antihistamines before the next infusion. They might also slow down the drip rate or switch to a different drug. Some patients need desensitization protocols—where tiny doses are given slowly over hours to train the body not to react. It’s not perfect, but it works for many.
And it’s not just about the drugs themselves. Some additives in chemo solutions—like polysorbate 80 or Cremophor EL—can also trigger reactions. These aren’t the active ingredients, but they’re needed to dissolve the medicine. If you’ve had an allergic reaction to a different drug with the same additive, your doctor needs to know.
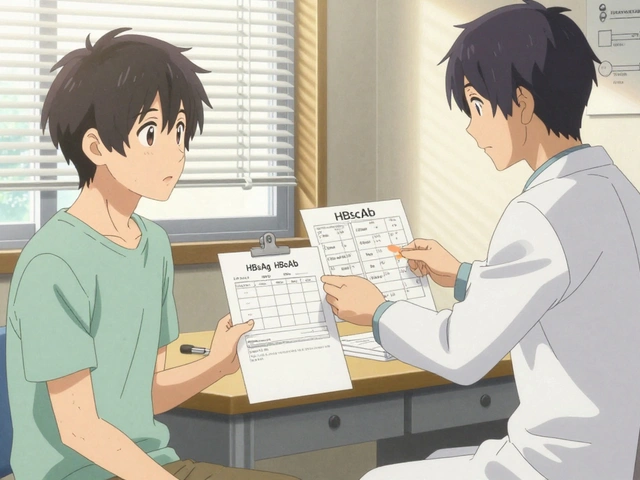
There’s no way to predict who will react, but knowing the signs saves lives. Keep a list of every chemo drug you’ve received, along with any side effects you had. Bring it to every appointment. If you’re ever given a new drug, ask: "Has this caused anaphylaxis in others? What’s the plan if I react?" You’re not being difficult—you’re being smart.
The good news? Most people never have this reaction. But for those who do, being prepared makes all the difference. Hospitals carry epinephrine auto-injectors for emergencies, and staff are trained to act fast. Still, your awareness is the first line of defense. If you’ve ever wondered why your nurse watches you so closely during chemo, now you know. It’s not routine—it’s lifesaving.
Below, you’ll find real patient stories, drug-specific risk profiles, and practical steps to reduce your chances of a reaction—so you can focus on healing, not worrying.
Chemotherapy hypersensitivity reactions can range from mild rashes to life-threatening anaphylaxis. Learn the signs, timing, and emergency protocols every patient and caregiver should know.
Nov 16 2025

Jan 1 2026
Dec 11 2025
Oct 20 2025

Dec 22 2025