Post-Operative Insomnia Assessment Tool
Assessment Parameters
Complete the following questions to get personalized insights on managing post-operative insomnia.
Your Assessment Results
When patients emerge from surgery, post‑operative insomnia is a common but often overlooked challenge. It refers to difficulty falling or staying asleep during the days following an operation. Sleep loss can slow wound healing, increase pain perception, and even raise the risk of complications. The good news? A mix of simple habits, targeted therapies, and environment tweaks can turn a restless night into a restorative one.
Why insomnia spikes after surgery
Two main forces collide during the early recovery phase. First, anesthesia agents disrupt the brain’s natural sleep‑wake circuitry, temporarily flattening the normal circadian rhythm. Second, postoperative pain, nausea, and the hospital’s 24‑hour buzz keep the body on high alert. Studies from the Royal College of Nursing in 2023 showed that up to 46% of patients report poor sleep quality in the first 48hours after major surgery.
Assessing sleep problems in the recovery ward
Before jumping to solutions, clinicians need a quick snapshot of the patient’s sleep status. Use a brief questionnaire that asks about:
- Time taken to fall asleep (sleep latency)
- Number of awakenings
- Overall sleep quality on a 0‑10 scale
- Use of rescue sleep medication
Document the answers in the electronic notes; trends over the first three nights often predict longer‑term issues.
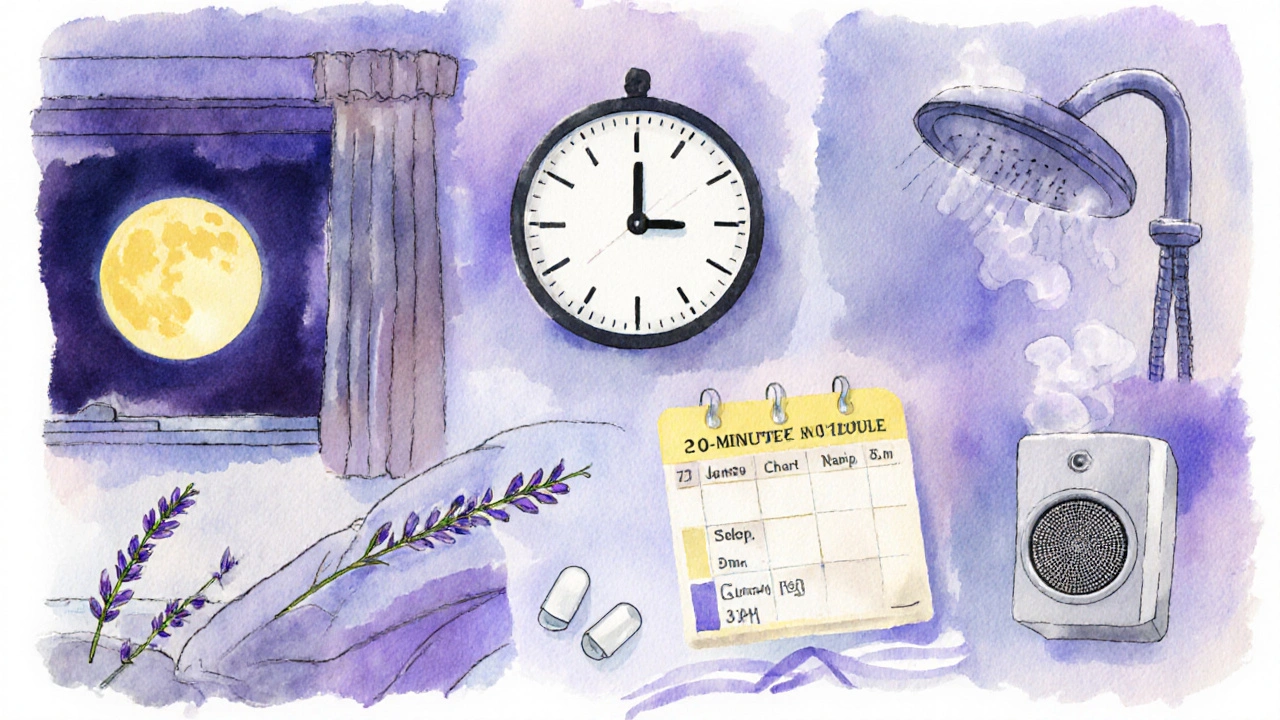
Non‑pharmacologic sleep strategies
Sleep hygiene refers to habits that promote natural sleep cycles is the first line of defence. Here are the most effective tweaks for a post‑surgical patient:
- Light control: Dim lights after 8p.m. and keep a low‑intensity night‑lamp for bathroom trips.
- Noise reduction: Offer earplugs or white‑noise machines; many wards now provide bedside speakers.
- Temperature: Aim for a room temperature of 18‑20°C; cool environments boost melatonin release.
- Scheduled rest: Encourage a short, 20‑minute nap before 3p.m. if fatigue is extreme, but avoid long daytime sleep.
When habits alone aren’t enough, Cognitive Behavioral Therapy for Insomnia (CBT‑I) is a short‑term, evidence‑based program that reshapes thoughts and behaviours around sleep can be delivered via a tablet in the ward. A 2022 trial in the UK showed a 30% reduction in insomnia severity scores after just three CBT‑I sessions.
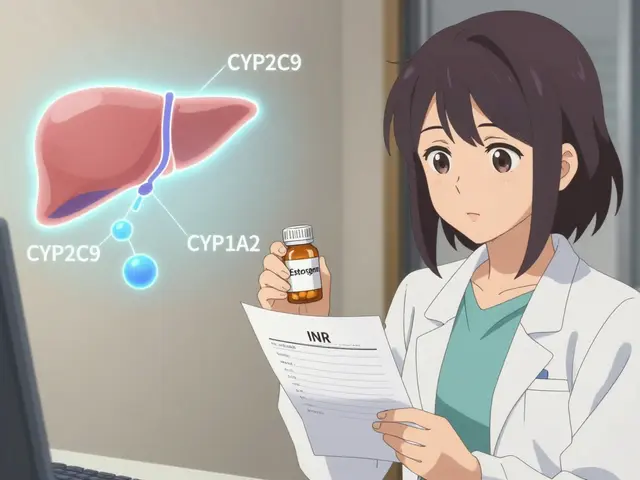
Pharmacologic options and safety
Pharmacologic sleep aids include short‑acting hypnotics and certain antihistamines used to induce sleep should be reserved for patients who cannot achieve rest despite non‑drug measures. Key considerations:
- Z‑drugs (e.g., zolpidem): Fast onset, but risk of respiratory depression if combined with opioids.
- Low‑dose trazodone: Useful for patients already on antidepressants; minimal impact on breathing.
- Melatonin: Mimics the body’s natural hormone, safe across most age groups, and especially helpful for night‑shift workers.
Always check renal and hepatic function before prescribing, and limit use to no more than three consecutive nights to avoid tolerance.
Tailoring pain control to protect sleep
Uncontrolled pain is a surefire way to keep the brain in “alert” mode. Aligning analgesia with sleep goals means:
- Choosing multimodal analgesia (acetaminophen+NSAID+regional block) to lower opioid doses.
- Scheduling opioid doses at least 4hours before bedtime, then tapering to a low‑dose rescue dose if needed.
- Monitoring for opioid‑induced sleep‑disordered breathing, especially in patients with obstructive sleep apnea.
Effective pain relief not only eases the surgical wound but also paves the way for deeper, uninterrupted sleep.
Optimising the recovery environment
Environmental modifications cover changes to lighting, sound, and comfort that support natural sleep cycles are simple yet powerful. Hospitals are rolling out “quiet hours” between 10p.m. and 6a.m., but patients can still take charge:
- Ask staff to cluster nighttime care activities (vitals, medication) to minimise interruptions.
- Use a bedside sleep mask to block residual light.
- Keep personal items like a familiar pillow or blanket; sensory comfort reduces stress hormones.
These tweaks cost almost nothing but have been shown to improve sleep efficiency by up to 15% in a 2024 NHS quality improvement project.

Creating a personalized sleep plan
After gathering data on pain levels, medication regimen, and sleep habits, draft a bedside checklist that the patient and nursing team can follow each night. A typical plan might read:
- 6p.m. - Light snack, stop caffeine, dim lights.
- 7p.m. - Warm shower, apply lavender scent.
- 7:30p.m. - Review pain meds; administer scheduled dose.
- 8p.m. - Start white‑noise machine, set room temperature.
- 8:15p.m. - Bedtime; optional melatonin 1mg.
- During night - Use earplugs, avoid screen use, call nurse only for urgent needs.
Review the plan each morning; adjust based on how the patient reports sleep quality. The iterative approach keeps the strategy patient‑centred and adaptable.
Quick reference: non‑pharmacologic vs pharmacologic approaches
| Approach | Onset | Side‑effects | Typical duration of use | Best for |
|---|---|---|---|---|
| Sleep hygiene & environment | Immediate | None | Ongoing | All patients |
| CBT‑I (digital) | 1‑2weeks | Mild frustration (homework) | 4‑6weeks | Persistent insomnia |
| Melatonin | 30minutes | Rare drowsiness next day | Up to 2weeks | Circadian misalignment |
| Z‑drugs (zolpidem) | 15‑30minutes | Residual sedation, falls | ≤3nights | Acute severe insomnia |
| Trazodone low‑dose | 1‑2hours | Orthostatic hypotension | Up to 1week | Patients on antidepressants |
Frequently Asked Questions
How long does post‑operative insomnia usually last?
For most patients the problem eases within a week as anesthesia wears off and pain is controlled. If sleep disruption persists beyond 10days, consider a formal sleep evaluation.
Is it safe to combine melatonin with my pain medication?
Melatonin has a low interaction profile and is generally safe with acetaminophen, NSAIDs, and even low‑dose opioids. Still, check with the prescriber if you’re on high‑dose opioids or sedatives.
Can I use my phone’s blue‑light filter at night in the hospital?
Yes, but keep the screen dim and limit use to under 15minutes. Blue‑light filters reduce melatonin suppression, helping the body wind down.
What if I’m already on a sleep medication before surgery?
Inform the anaesthetic team. They may adjust intra‑operative drugs to avoid additive sedation and plan a taper schedule for the postoperative period.
Are there any non‑drug tricks to fall asleep faster after surgery?
Yes - a warm shower, gentle breathing exercises, and a brief 10‑minute mindfulness session have all been shown to cut sleep latency by 5‑10minutes in recovery cohorts.





Comments
Annette Smith
Good points about dimming lights after surgery.
beth shell
Sleep hygiene is often underrated it can make a big difference in recovery the simple steps are easy to follow and cheap to implement many patients benefit from a calm environment.
khushali kothari
The postoperative period represents a critical nexus of neurophysiological perturbations that predispose patients to fragmented sleep architecture.
Anesthetic agents, particularly volatile inhalational compounds, attenuate the homeostatic drive for slow-wave sleep by modulating GABAergic transmission.
Concurrently, nociceptive signaling amplifies cortical arousal via the locus coeruleus, thereby compromising REM latency.
Quantitative polysomnographic studies have demonstrated a 30% reduction in total sleep time within the first 48 hours post‑incision.
Moreover, the dysregulation of melatonin secretion observed in peri‑operative cohorts underscores the circadian misalignment inherent to surgical stress.
Implementing multimodal analgesia, incorporating acetaminophen, NSAIDs, and regional blocks, attenuates nociceptive input and mitigates sleep disruption.
Non‑pharmacologic interventions, such as controlled ambient lighting and acoustic dampening, serve to reinforce the endogenous suprachiasmatic rhythm.
The utilization of white‑noise generators has been empirically associated with a 12% increase in sleep efficiency in controlled trials.
In patients with pre‑existing obstructive sleep apnea, titration of opioid dosing is paramount to avoid central hypoventilation.
Pharmacologic adjuncts, including low‑dose trazodone and exogenous melatonin, should be prescribed contingent upon hepatic and renal function parameters.
Recent meta‑analyses corroborate that a three‑day course of melatonin yields statistically significant improvements in sleep latency without deleterious respiratory effects.
Cognitive behavioral therapy for insomnia, delivered via digital platforms, facilitates neurocognitive restructuring and has demonstrated durability of effect at six‑month follow‑up.
Environmental stewardship, exemplified by scheduled nighttime vitals clustering, reduces nocturnal interruptions and preserves sleep continuity.
A bedside checklist operationalizing these modalities can be integrated into electronic health records to promote adherence.
Ultimately, a synergistic approach that aligns analgesic optimization with circadian supportive strategies constitutes best practice for postoperative sleep management.
Brandon Smith
While the guide is thorough, it neglects the fundamental responsibility of clinicians to prioritize sleep as a vital sign. Overlooking this can lead to preventable complications.
Alexander Rodriguez
These tips are solid and easy for patients to follow.
Bailee Swenson
Honestly, if you don’t start using these right away, you’re just prolonging your suffering 😤💤.
tony ferreres
Great summary! 🌟 Remember, every patient’s needs differ, so tailor the plan accordingly.
Krishna Chaitanya
Whoa! The room turned into a battlefield of beeping monitors and endless lights-totally ruined any chance of peaceful sleep!
Sarah Hoppes
They don’t want us to know the real reason hospitals sabotage sleep.
Robert Brown
False. Hospitals try to keep patients awake for profit.
Erin Smith
Love the positive vibe here, it really lifts the mood for anyone recovering.
George Kent
Indeed, the recommendations are scientifically sound; however, one must ensure that the dosage of melatonin does not exceed recommended limits, as excessive intake may cause dysregulation of endogenous rhythms.
Jonathan Martens
Ah, another masterpiece of evidence‑based protocol-because nothing screams “cutting‑edge” like a checklist that could double as a spreadsheet for the statistically inclined.
Jessica Davies
Sure, but let’s not pretend that a bedside checklist isn’t just a bureaucratic band‑aid that masks the deeper issue of institutional neglect.
Lynnett Winget
Keep experimenting with bright lavender scents and cozy blankets; creativity fuels healing and makes those sleepy nights feel like a warm hug.