When you pick up a prescription for insulin or a biologic drug like Humira, you might not realize your pharmacist could swap it for a cheaper version without telling you. That’s not a mistake - it’s the law in many states, thanks to something called interchangeability. But this isn’t like swapping one generic pill for another. Biosimilars are far more complex, and the rules around who can switch them, when, and why are anything but simple.
What Makes a Biosimilar Interchangeable?
Not all biosimilars are created equal. The FDA approves two types: biosimilars and interchangeable biosimilars. Both are highly similar to the original biologic drug - think Humira, Enbrel, or Lantus. But only one type can be swapped automatically at the pharmacy counter.
To get that interchangeability stamp, a company doesn’t just prove the biosimilar works like the original. They have to prove you can switch back and forth between them - multiple times - without any added risk. That means clinical studies where patients alternate between the reference drug and the biosimilar, sometimes several times over weeks or months. The FDA looks for no drop in effectiveness, no rise in side effects, and no immune reactions triggered by the switches.
This is a huge hurdle. A regular generic drug, like simvastatin, is a simple chemical copy. You can make it in a lab, and it’s identical to the brand. Biosimilars are made from living cells - think yeast or hamster ovary cells. Tiny changes in the process can affect how the drug behaves in your body. That’s why the FDA requires extra proof before allowing automatic substitution.
As of November 2023, the FDA has approved 41 biosimilars. Only 10 of them carry the interchangeable label. The first was Semglee, an insulin glargine product approved in July 2021. The first interchangeable monoclonal antibody - the same class as Humira - was Cyltezo, approved in August 2023.
Why Does This Matter for Patients?
Cost. Plain and simple.
Biologics are among the most expensive drugs in the world. Humira, for example, cost over $7,000 a month before biosimilars entered the market. Interchangeable biosimilars can cut that price by 15% to 30%, according to a 2022 RAND Corporation study. That’s thousands of dollars a year in savings.
For patients on long-term treatments - like those with rheumatoid arthritis, psoriasis, or Crohn’s disease - that kind of savings can mean the difference between staying on treatment and skipping doses due to cost.
But here’s the catch: you might not know it happened. In states that allow automatic substitution, pharmacists can swap your Humira for Cyltezo without calling your doctor. Some patients don’t mind. One user on the Psoriasis Foundation forum wrote, “I saved $800 a month with no change in how I feel.”
Others aren’t so lucky. Another patient reported an adverse reaction after a pharmacy switched them to Hadlima without warning. Turns out, they were allergic to an inactive ingredient - something that wasn’t obvious from the label. The FDA says all approved biosimilars are safe and effective, but even tiny differences in formulation can cause reactions in sensitive individuals.
State Laws Are a Mess
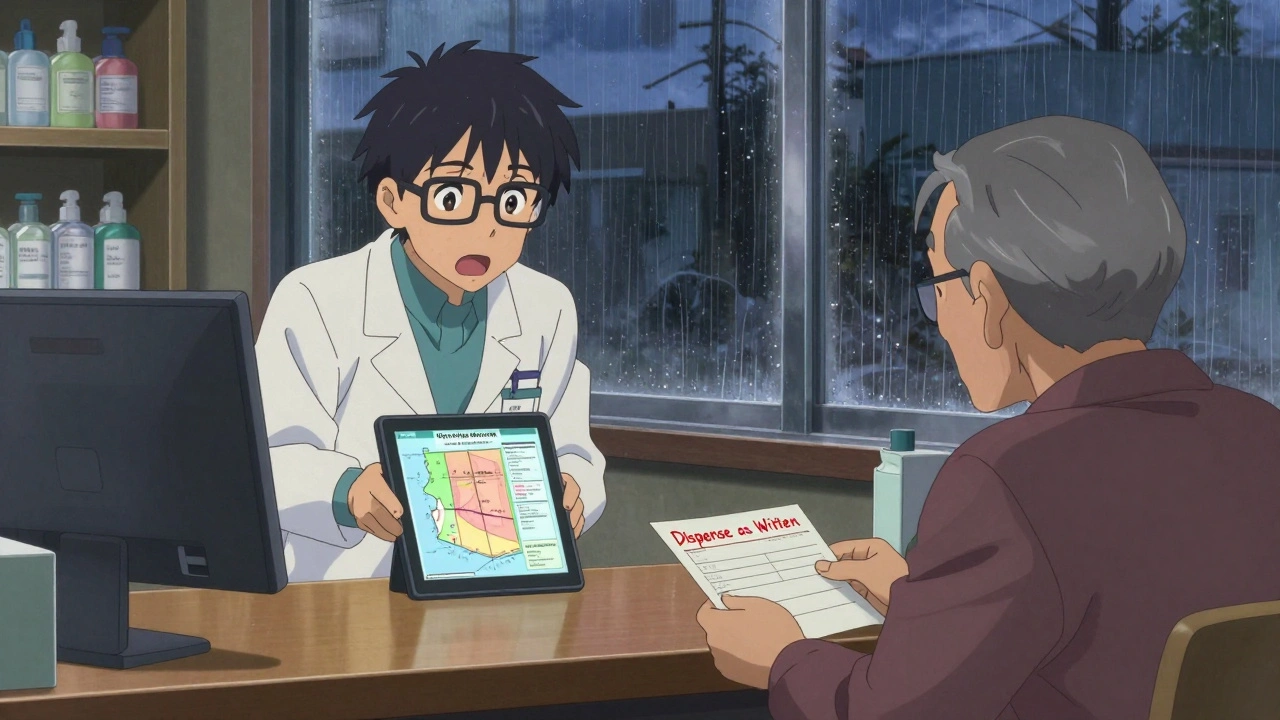
Just because the FDA says a biosimilar is interchangeable doesn’t mean your pharmacist can swap it. That decision is made at the state level - and every state has its own rules.
Forty states let pharmacists substitute interchangeable biosimilars without asking the prescriber. Arizona, for example, has had this law since 2016. But in those states, pharmacists still have to notify you, record the exact product dispensed, and send that info to your doctor within five days. They also have to keep those records for seven years.
Then there are the exceptions. Four states - Alabama, Indiana, South Carolina, and Washington - require your doctor’s permission before any substitution can happen. Six states and Washington, D.C. only allow substitution if it saves you money. That means if your insurance already covers the brand-name drug at a low copay, your pharmacist can’t switch you - even if the biosimilar is cheaper.
This patchwork creates chaos for pharmacies. A 2022 survey by the National Community Pharmacists Association found that 67% of independent pharmacists felt confused about what they could and couldn’t do depending on the patient’s state. One pharmacist on Reddit wrote: “In California, I have to check if it’s lower cost. In Arizona, I don’t. My system doesn’t tell me which state the patient lives in.”

What About Other Countries?
The U.S. is the only country with this formal “interchangeable” designation. In the European Union, biosimilars are approved, but substitution is up to the doctor or pharmacist - no automatic swaps. Canada lets Health Canada label a biosimilar as interchangeable, but provinces decide whether to allow the swap. Japan requires extra clinical data but doesn’t use the term “interchangeable” at all.
That means if you’re traveling or moving, your biosimilar might not be interchangeable - or even available - in another country. The U.S. system is unique, and it’s still evolving.
Who’s Winning and Who’s Losing?
Patients and payers are mostly on the same side: lower cost, better access. A 2023 JAMA Health Forum study showed that states with automatic substitution laws saw 18.7% higher use of biosimilars for insulin. Semglee, the first interchangeable insulin, grabbed 17.3% of the market within six months - more than double the uptake of non-interchangeable biosimilars.
But not everyone’s happy. Some doctors worry about treatment disruption. A 2021 JAMA Dermatology editorial noted that psoriasis patients switched to biosimilars had a 20.3% higher chance of stopping treatment altogether - possibly because of side effects or lack of trust in the change.
Pharmaceutical companies that make the original biologics argue that switching without consent could hurt patient outcomes. The PhRMA group opposes efforts to make all biosimilars interchangeable without switching studies. On the other side, the Biosimilars Council says the current rules are just red tape holding back savings.
There’s even a bill in Congress - the Biosimilar Red Tape Elimination Act - that wants to scrap the switching studies entirely. If it passes, every FDA-approved biosimilar could become automatically interchangeable. Critics say that’s dangerous. Supporters say it’s long overdue.
What Should You Do as a Patient?
Don’t assume your drug was switched. Ask your pharmacist. If you’re on a biologic, make sure you know exactly what you’re getting - brand name, biosimilar, or interchangeable biosimilar. Check the label. Ask if it’s been changed.
Also, tell your doctor if you notice any new side effects after a switch. Even if it’s minor - a rash, fatigue, or joint pain - it could be a sign your body is reacting to something different in the formulation.
If you’re concerned about automatic substitution, ask your doctor to write “Dispense as Written” on your prescription. That blocks any swap, no matter what state you’re in.
And if you’re confused? You’re not alone. The Arthritis Foundation’s “Biosimilars 101” guide has been downloaded over 47,000 times. Patient education is still catching up.
What Pharmacists Need to Know
Pharmacists are on the front lines. They’re the ones holding the bottle, scanning the barcode, and deciding whether to swap. But they’re also drowning in rules.
They need to know:
- Which biosimilars are FDA-designated as interchangeable
- What their state law allows - and doesn’t allow
- Whether insurance requires substitution
- How to document the swap properly
- How to communicate the change to the patient and prescriber
The American Pharmacists Association has trained over 12,000 pharmacists through its Biosimilars Certificate Program. Still, a 2023 survey found pharmacists spend nearly 9 hours a year just keeping up with the rules.
It’s not just about science. It’s about paperwork, communication, and legal compliance - all while managing a busy pharmacy.
The Future Is Unclear - But Moving Fast
By 2025, 70% of the top 20 biologic drugs will have biosimilar competition. That’s billions of dollars in savings waiting to be unlocked. But only if the system works.
Right now, the U.S. has the most advanced regulatory framework for biosimilar substitution - but also the most complicated. Patients benefit from lower prices, but they also face confusion and potential risk. Pharmacists are caught in the middle. Doctors worry about continuity of care.
The next big shift might come from Congress. If the Biosimilar Red Tape Elimination Act becomes law, we could see all biosimilars treated as interchangeable - no switching studies needed. That could speed up access and lower costs even more. But it could also remove safeguards that protect sensitive patients.
One thing is certain: automatic substitution isn’t going away. The question isn’t whether it will happen - it’s how well we can make it safe, clear, and fair for everyone involved.
Can any biosimilar be swapped automatically at the pharmacy?
No. Only biosimilars that have received an official "interchangeable" designation from the FDA can be swapped without the prescriber’s approval. Most biosimilars are not interchangeable - they still require a doctor’s permission to substitute. As of late 2023, only 10 out of 41 approved biosimilars have this status.
Is an interchangeable biosimilar safer or more effective than a regular biosimilar?
No. Both interchangeable and non-interchangeable biosimilars meet the same FDA standards for safety, purity, and effectiveness. The only difference is that interchangeable biosimilars have passed extra studies showing you can switch back and forth between them and the original drug without increased risk. The designation is about substitution logistics, not quality.
Can my pharmacist switch my biologic without telling me?
In most states, yes - but they’re required to notify you. Even in states that allow automatic substitution, pharmacists must inform you that a switch happened, record the product dispensed, and send details to your doctor. However, some patients report not being told at all. Always check your prescription label and ask if anything changed.
What if I have an adverse reaction after a biosimilar switch?
Contact your doctor immediately. While rare, reactions can happen due to differences in inactive ingredients - things like preservatives or stabilizers - not the active drug. These aren’t always listed clearly on the label. Document what happened and ask your doctor to note "dispense as written" on future prescriptions to prevent future switches.
Are biosimilars covered by insurance the same way as brand-name biologics?
Most commercial health plans require automatic substitution for interchangeable biosimilars when allowed by state law. Many insurers have stepped up their incentives, making biosimilars the lowest-cost option. But coverage rules vary - some plans still favor the brand-name drug unless you or your doctor request a switch. Always check your plan’s formulary before assuming a biosimilar will be covered.





Comments
Nikhil Pattni
Look, I get that biosimilars save money, but let’s be real-these aren’t like generics. I work in pharma logistics in India, and I’ve seen how even minor changes in cell culture conditions can alter glycosylation patterns in monoclonal antibodies. That’s not just a tweak; it’s a biological wildcard. The FDA’s interchangeability criteria? Fine on paper, but real-world immunogenicity? We’re talking about patients who’ve been stable on Humira for a decade suddenly getting rashes or joint flares because some batch from a different facility had a 0.3% shift in sialic acid content. And don’t get me started on how pharmacists don’t even know what’s in their own inventory half the time. 😒
precious amzy
One is tempted to posit that the entire regulatory architecture surrounding biosimilars is less a function of clinical necessity and more a manifestation of neoliberal market imperatives masquerading as patient-centric policy. The notion of 'interchangeability'-a term laden with epistemological ambiguity-functions as a rhetorical device to legitimize cost-cutting under the guise of therapeutic equivalence. The patient, in this schema, is reduced to a mere unit of consumption, their biological singularity erased in the name of fiscal efficiency. One must ask: at what cost does access come?
Courtney Black
It’s not about safety. It’s about trust. If you’ve been on the same biologic for years, your body adapts. Switching without warning? It’s like changing your therapist because the new one is cheaper. You don’t know if it’s the drug or the switch that made you feel off. And no, the label doesn’t help. I’ve read them. They’re written in legalese for lawyers, not patients.
Richard Eite
USA is the only country that gets this right. Europe? They’re still stuck in the 2000s. Canada? Half-baked. Japan? Too cautious. We have the science, the regulation, the innovation. Stop whining about 'risk'-if you can’t handle a biosimilar, you shouldn’t be on a biologic in the first place. Save your money, stop being a baby, and let the market work. #AmericanExceptionalism
Gilbert Lacasandile
I’ve been a pharmacist for 18 years and I’ll tell you this: the real issue isn’t the science. It’s the paperwork. I’ve got five different state rules to juggle, three insurance formularies, and a system that doesn’t even flag the patient’s state of residence. I once swapped a patient’s insulin because I thought they were from Arizona-turns out they were visiting from Alabama. Got a call from their doctor the next day. I spent three hours filling out forms just to fix it. No one trains us for this. No one cares.
Lola Bchoudi
From a clinical operations standpoint, the real bottleneck isn’t interchangeability-it’s the lack of interoperable EHR integration. If the pharmacy’s dispensing system can’t auto-populate the product’s NDC, the prescriber’s notification protocol fails, and the patient’s longitudinal data becomes fragmented. We need standardized FHIR-based triggers for substitution events, mandatory patient-facing alerts via portal, and closed-loop communication with prescribers. Without this, we’re just adding administrative entropy to an already complex ecosystem.
Morgan Tait
Ever wonder why Big Pharma doesn’t want you to know this? The original biologics are cash cows-$20 billion a year for Humira alone. Biosimilars? They’re the Trojan horse. The FDA’s 'interchangeable' label? A backdoor for generics to sneak in under the guise of science. And don’t think they’re not lobbying Congress to gut the switching studies. They’ve got lobbyists in DC wearing lab coats. I’ve seen the emails. They’re not trying to help you-they’re trying to kill competition. Stay vigilant. Check your bottle. Ask questions. They don’t want you to.
Darcie Streeter-Oxland
It is, perhaps, an understatement to observe that the current regulatory framework governing the substitution of biosimilars is characterised by a profound dissonance between the stated objective of cost containment and the actual operational realities faced by frontline healthcare providers. The heterogeneity of state legislation, coupled with the absence of a unified national standard, engenders a labyrinthine environment wherein pharmacists are compelled to navigate a patchwork of conflicting mandates. This, in turn, compromises the integrity of patient care.
Chris Marel
Just wanted to say thank you for writing this. I’m from Nigeria and we don’t even have biosimilars approved yet. My cousin’s on Humira and her family spends half their income on it. I showed this to her doctor and now she’s asking about access. I just hope when it comes here, we don’t repeat the same mistakes. Maybe we can build something better-clearer rules, better patient education, no surprise switches. Thanks for making me care about this.