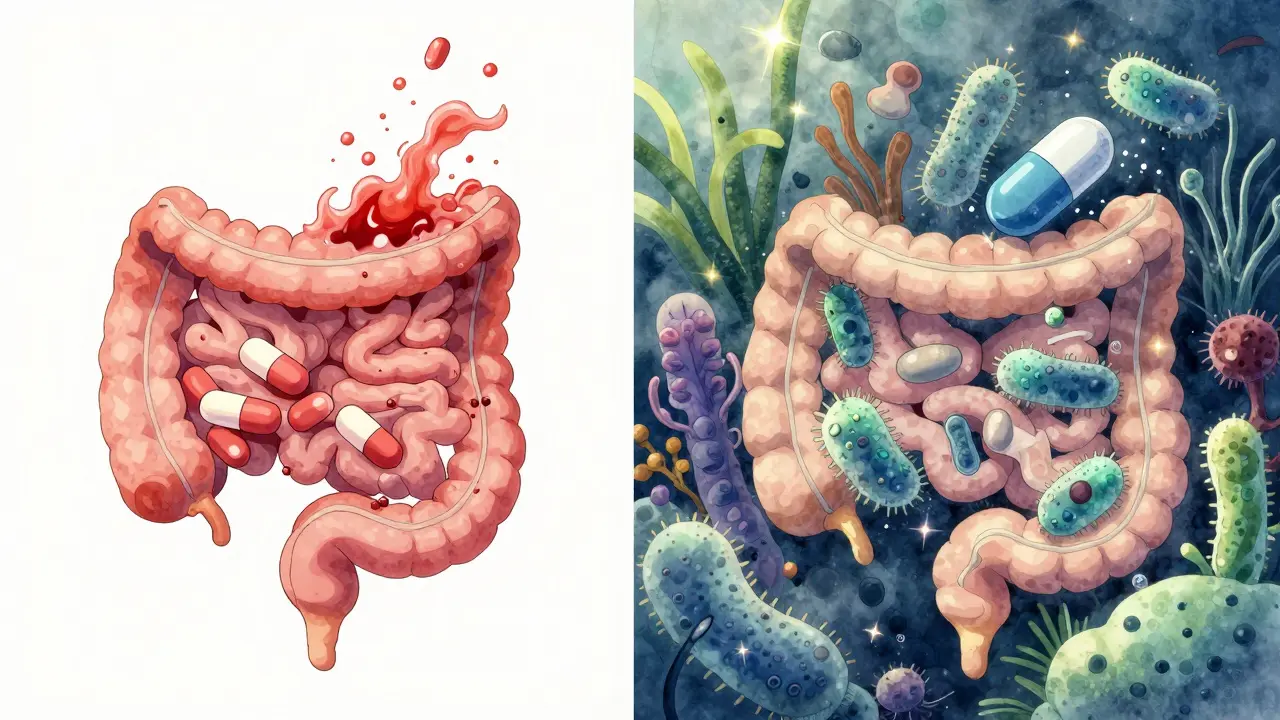
When you’re on antibiotics, your gut knows it. The good bacteria, the ones that help with digestion, immunity, and even mood, get wiped out along with the bad ones. That’s why so many people end up with bloating, cramps, or worse - antibiotic-associated diarrhea. About 30% of people on antibiotics get it. But there’s a simple fix that most people don’t do right: taking probiotics at the right time.
Why Timing Matters More Than the Brand
You can buy the most expensive probiotic with 50 strains and 100 billion CFUs, but if you swallow it right after your antibiotic pill, it’s basically dead on arrival. Antibiotics don’t care if a microbe is good or bad - they kill bacteria. And most probiotics? They’re bacteria. So if you take them together, the antibiotic kills the probiotic before it even gets a chance to settle in your gut. The science is clear: you need to space them out. At least two hours. That’s not a suggestion. It’s the minimum window needed for the antibiotic to move through your system before the probiotic shows up. Studies show that taking probiotics within two hours of an antibiotic reduces their survival rate by 78-92%. That’s not just less effective - it’s almost useless.What’s the Right Schedule?
Let’s say you’re on amoxicillin twice a day - 8 a.m. and 8 p.m. Here’s what your day should look like:- 6 a.m. - Probiotic
- 8 a.m. - Antibiotic
- 10 a.m. - Probiotic (if you’re doing a second dose)
- 6 p.m. - Probiotic
- 8 p.m. - Antibiotic
- 10 p.m. - Probiotic (if needed)
Not All Probiotics Are the Same
Here’s where most people get confused. Not every probiotic needs to be spaced out. Saccharomyces boulardii is a yeast, not a bacterium. Antibiotics don’t kill yeast. That means you can take it at the same time as your antibiotic without losing effectiveness. In fact, it’s one of the most studied strains for preventing antibiotic-associated diarrhea. Research shows it cuts your risk by 52% when taken at 20 billion CFUs per day. For bacterial probiotics - like Lactobacillus rhamnosus GG or Bifidobacterium strains - spacing is non-negotiable. LGG alone has been shown to reduce diarrhea risk by 47% in adults. But only if you give it time to survive.How Much Should You Take?
Dose matters. A little won’t cut it. You need enough good bacteria to outlast the antibiotic chaos.- 5-10 billion CFUs - for short courses (3-5 days) and mild symptoms
- 10-20 billion CFUs - for moderate diarrhea or longer courses (7-14 days)
- 20-40 billion CFUs - for severe gut disruption, broad-spectrum antibiotics, or if you’ve had issues before
How Long Should You Keep Taking Them?
Don’t stop when the antibiotic bottle is empty. Your gut needs time to rebuild. Most studies show that taking probiotics for just the duration of the antibiotic course isn’t enough. You need to keep going. The gold standard? Continue for 7 to 14 days after your last antibiotic pill. One study found that people who did this had 89% microbiome recovery. Those who stopped early? Only 63%. And yes - even if you feel fine. You’re not just preventing diarrhea. You’re preventing long-term imbalance that can lead to bloating, food sensitivities, or even recurring infections.What If You Forget?
Life happens. You miss a dose. You take your probiotic 30 minutes after your antibiotic. It’s not the end of the world. But if you do it often, it adds up. One study found that skipping just one probiotic dose per week cut effectiveness by 37%. So if you’re going to do this, do it consistently. Set phone alarms. Use pill organizers. Write it on your calendar. This isn’t optional - it’s the difference between your gut bouncing back or staying off-kilter for months.What About the New Time-Release Probiotics?
You’ve probably seen ads for “antibiotic-resistant” probiotics or time-release capsules. Companies like Seed and Pendulum are developing acid-coated pills that claim to protect the bacteria until they reach your intestines. That sounds great - and it might help. But here’s the catch: no product has been proven to eliminate the need for spacing. The 2-hour rule still holds. Even the best capsules can’t fully shield bacteria from high concentrations of antibiotics in the gut. Until more long-term human trials come out, stick with the proven method: time it right.







Comments
Chloe Hadland
Just took amoxicillin yesterday and forgot to space my probiotic. Now I’m paying for it with bloating that feels like I swallowed a balloon. Lesson learned. Thanks for the clear guide.
Marie-Pier D.
OMG YES. I used to take mine together like a dumbass 🙈 Now I set two alarms-one for the antibiotic, one for the probiotic. My gut hasn’t complained in months. You’re a lifesaver, truly 💕
Shelby Marcel
i read this whole thing and still dont know if i should take it before or after my coffee. like… is coffee bad? help.
Alexandra Enns
Wow. Another ‘science’ post from someone who thinks ‘studies show’ means they read a blog. Did you even check if those CFU numbers are clinically validated or just marketing fluff? I’ve seen 3 different meta-analyses that say probiotics do jack squat for antibiotic diarrhea unless you’re in a hospital. And Saccharomyces boulardii? That’s a fungus. You’re not ‘saving your gut’-you’re feeding yeast. My cousin in Toronto got candida from this exact advice. Don’t turn your intestine into a cult.
Patrick Gornik
Let’s deconstruct the metaphysics of microbial hegemony here. The antibiotic isn’t ‘killing’-it’s enforcing a colonial order on the gut’s microbiotic democracy. The probiotic, a subversive organism, seeks to reestablish equilibrium through nonviolent resistance. But when you space them two hours apart, you’re not preserving life-you’re institutionalizing a temporal ceasefire. The real question: Are we treating the body as a battlefield… or as a biosphere? And if it’s the latter, why are we still using war metaphors? The answer lies not in CFUs, but in epistemic humility.
Amelia Williams
I switched to S. boulardii after my last round of clindamycin and I swear my gut went from ‘war zone’ to ‘spa day’. No more cramps, no more panic at the bathroom door. And I took it with my breakfast-no spacing. Maybe I got lucky? But I’m not complaining. This stuff is magic.
Tommy Sandri
While the recommendations presented are generally aligned with current clinical guidelines, one must acknowledge the heterogeneity of gut microbiota across populations. The efficacy of Lactobacillus rhamnosus GG, for instance, may vary significantly in individuals of East Asian descent due to dietary and genetic factors. Further, the notion of a universal dosing protocol may overlook individual variability in gastric emptying time. A more personalized approach, informed by microbiome sequencing, may be warranted in the future.
Karen Conlin
Thank you for this. I’m a nurse and I’ve seen so many patients stop probiotics the day they finish antibiotics. They think ‘I feel fine’ = ‘I’m fixed’. Nope. Your gut is rebuilding like a city after a hurricane. You don’t stop sending supplies just because the sirens are gone. Keep going. Two weeks. Minimum. Your future self will thank you.
blackbelt security
Probiotics are a placebo wrapped in hype. Your gut doesn’t need a babysitter. It’s been surviving since the Paleolithic. Let it heal itself. You’re overcomplicating a natural process. Just eat yogurt. Real yogurt. Not that lab-made crap.
Phil Maxwell
I’ve been doing the 2-hour thing for 3 months now. Still not sure if it’s working, but at least I’m not having diarrhea. So… progress? I guess.
Luke Davidson
Just read this after my doc prescribed me a 14-day course of amoxicillin. I’ve been taking probiotics for years but never spaced them. I’m gonna try this schedule for real now. Honestly? I’m scared my gut’s gonna revolt. But if it works, I owe you a coffee 🤝
Sushrita Chakraborty
Thank you for the detailed and scientifically accurate explanation. I particularly appreciate the emphasis on strain specificity and the warning against generic brands. In India, probiotics are often marketed as ‘miracle pills’ without any strain information-this clarity is desperately needed.
Patrick Gornik
Interesting. So you’re telling me that the 2-hour rule is based on pharmacokinetic models from the 1980s, but we’ve never done a controlled trial comparing spaced vs. simultaneous administration in real-world populations with diverse microbiomes? Then it’s not science-it’s protocol inertia. We’re clinging to a ritual because it sounds rational. But rationality ≠ effectiveness. What if the real issue is antibiotic duration? Or diet? Or stress? Maybe we’re just blaming the probiotic timing to avoid confronting the systemic failures of our medical model.
Karen Conlin
And that’s why we have clinical guidelines-because real people aren’t lab rats. We don’t wait for perfect studies to help someone with diarrhea. We use what works. And it works. I’ve watched patients go from bedridden to hiking again because they followed this. Your philosophy is beautiful. But your patient? They need a schedule, not a seminar.