Bisphosphonate Safety Checklist
Follow These Rules to Prevent Esophageal Damage
Proper dosing reduces esophageal irritation risk by up to 90%. Verify your compliance with these critical steps.
Your Checklist
Input Your Details
Your Risk Assessment
Compliance: 0%
No results yet
Important Safety Note
Even with 100% compliance, bisphosphonates can cause esophageal damage if you have pre-existing GERD or esophageal motility issues. Always discuss with your doctor.
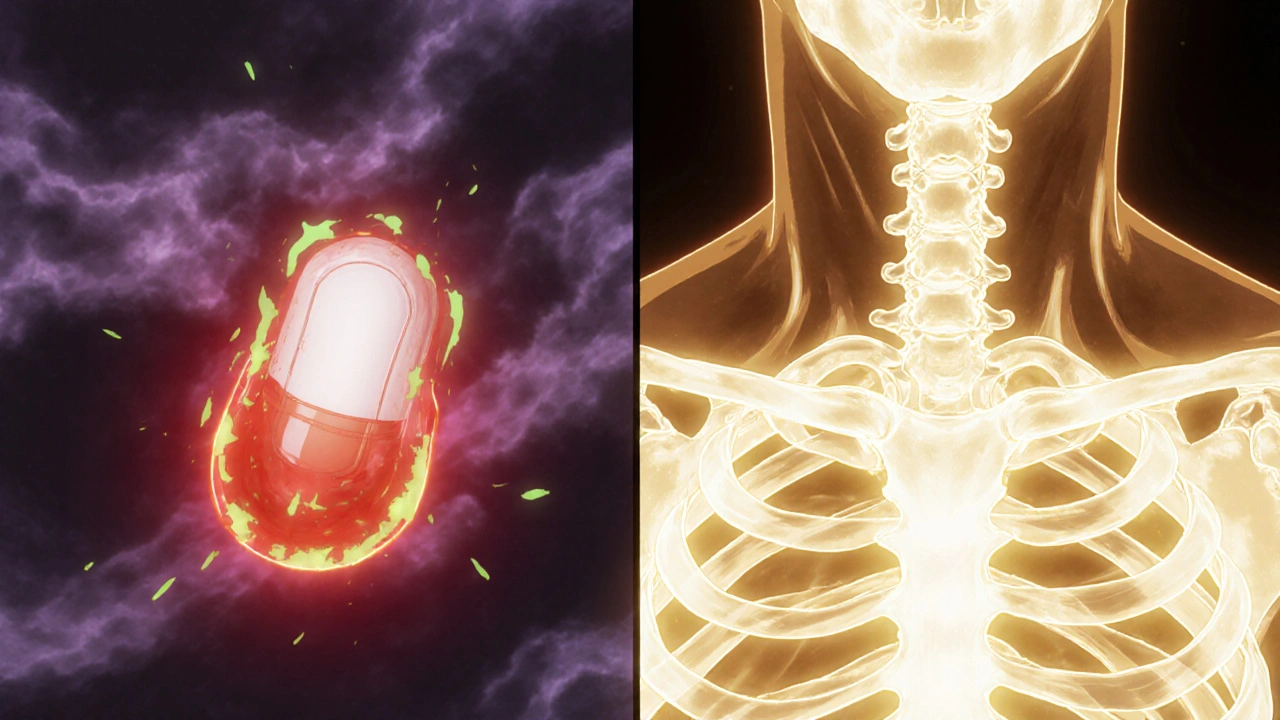
When you’re taking a medication to protect your bones, the last thing you want is for it to damage your esophagus. But for people with GERD, taking oral bisphosphonates like alendronate (Fosamax), risedronate (Actonel), or ibandronate (Boniva) can be a risky balancing act. These drugs are powerful - they cut fracture risk by up to 70% in osteoporosis patients - but they can also burn your esophagus if not taken correctly. And if you already have acid reflux, the danger is even higher.
Why Bisphosphonates Can Burn Your Esophagus
Bisphosphonates aren’t meant to sit in your esophagus. They’re designed to travel quickly to your bones. But when they get stuck - especially in someone with GERD - they can turn into a harsh acid that eats away at the lining. Alendronate, for example, changes form when stomach acid drops below pH 2.0. That’s when it becomes free acid, a chemical irritant that doesn’t care if you’ve got a healthy esophagus or one already inflamed from reflux.Studies show that about 0.7% of people taking alendronate develop esophagitis - inflammation or sores - compared to 0.4% on placebo. That might sound low, but for someone with chronic GERD, the risk jumps. One study found that patients with pre-existing esophageal motility issues or strictures were nearly five times more likely to suffer damage. And it’s not just rare cases. The FDA’s adverse event database recorded over 170 reports of esophageal toxicity linked to bisphosphonates between 2004 and 2023. Common symptoms? Difficulty swallowing, chest pain, heartburn that won’t quit, and a burning feeling behind the breastbone.
GERD Makes It Worse - Here’s Why
GERD isn’t just about heartburn. It means your lower esophageal sphincter is weak, letting stomach acid creep up. That acid doesn’t just cause discomfort - it slows down how fast pills move through your esophagus. When a bisphosphonate tablet lingers in an already irritated area, the damage multiplies. A 2023 study tracked a 72-year-old woman who took her alendronate tablet while lying down. Within days, she developed severe esophagitis and had to be hospitalized. Her case wasn’t unique.People with GERD often lie down after meals, nap after taking meds, or eat too close to bedtime. All of these habits increase the chance that the pill will get stuck. And if you’re already taking proton pump inhibitors (PPIs) for reflux, you’re not necessarily safe. In fact, 22.7% more GERD patients started PPIs after beginning bisphosphonates - a sign doctors were seeing more irritation and trying to manage it.
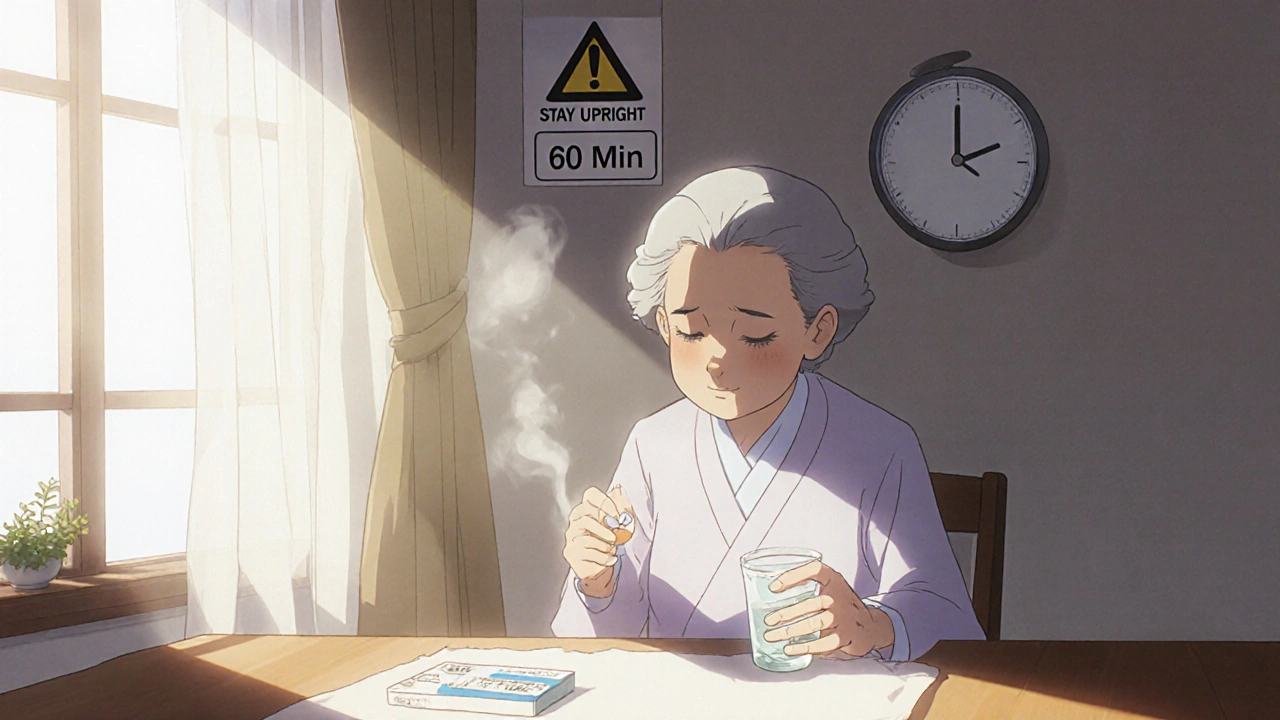
The Rules: How to Take Bisphosphonates Without Harming Your Esophagus
There’s one simple truth: how you take the pill matters more than the pill itself. If you follow the rules, your risk drops dramatically. Here’s what works:- Take it with a full glass of plain water - 6 to 8 ounces. Don’t use mineral water, juice, coffee, or tea. They can bind to the drug and slow its passage. Plain water is the only thing that reliably pushes the tablet down.
- Stay upright for at least 60 minutes after taking it. Sit or stand. Don’t lie down. Don’t recline. Don’t bend over. Don’t nap. The FDA updated its label in 2023 to require this 60-minute window - not 30. That’s because research showed 30 minutes wasn’t enough for some people.
- Wait until after your first meal to eat or drink anything else. Even a sip of water or a bite of toast too soon can trap the pill in your esophagus.
- Take it first thing in the morning. That gives you the whole day to stay upright. Taking it at night? That’s a recipe for trouble.
- Never take it with food or other meds. Calcium, iron, antacids, and even vitamins can block absorption. Take bisphosphonates on an empty stomach.
One patient on WebMD wrote: “I had terrible heartburn the first week. Then I started drinking 8oz of water and staying upright for an hour. It vanished.” That’s not luck - it’s science.
What If You Already Have GERD? Should You Even Take These Pills?
You don’t have to choose between broken bones and a damaged esophagus. There are alternatives - and your doctor should discuss them with you.Denosumab (Prolia) is a monthly injection that works just as well as bisphosphonates to prevent fractures, but it never touches your esophagus. No irritation. No reflux risk. The catch? It costs over $1,500 per dose, and you need to keep getting it - stop it, and your bone loss can accelerate.
Zoledronic acid (Reclast) is an IV infusion given once a year. It bypasses the esophagus entirely. But it can strain your kidneys, so it’s not for everyone - especially if you have existing kidney problems.
Teriparatide (Forteo) and romosozumab (Evenity) are other options. Teriparatide stimulates new bone growth, while romosozumab builds bone faster than bisphosphonates. But both are expensive - Evenity runs about $5,000 per month - and come with their own risks (like heart concerns with Evenity).
If you have severe GERD, strictures, or swallowing problems, your doctor may skip oral bisphosphonates entirely. A 2024 guideline from the American Gastroenterological Association recommends checking your esophageal motility with a pH test if symptoms persist despite perfect dosing.
When to Call Your Doctor
Not every bit of discomfort means disaster. But some signs need attention:- New or worsening chest pain that doesn’t feel like typical heartburn
- Feeling like food is stuck in your chest
- Pain when swallowing
- Vomiting blood or black, tarry stools
If you’re on a bisphosphonate and you notice any of these, stop the medication and call your doctor. Don’t wait. Endoscopic exams can show early damage before it becomes serious. And if you’ve been taking these pills for years, don’t assume you’re safe. Long-term use can cause silent damage - especially if your GERD has gotten worse over time.
Bottom Line: You Can Have Strong Bones Without a Damaged Esophagus
Bisphosphonates are still the most cost-effective osteoporosis treatment. Generic alendronate costs less than $1 per pill. That’s why they’re prescribed to 65% of new osteoporosis patients in the U.S. But cost shouldn’t override safety.If you have GERD, your treatment plan needs to be personalized. Talk to your doctor about your reflux history. Ask if you’re a good candidate for oral bisphosphonates - or if an injection might be safer. Follow the dosing rules exactly. Don’t cut corners. And if your symptoms don’t improve after changing how you take the pill, it’s time to reconsider the drug.
Strong bones matter. But so does your esophagus. You don’t have to choose one over the other - you just need to be smart about how you take your medicine.
Can I take bisphosphonates if I have GERD?
Yes, but only if you follow strict dosing rules: take the pill with a full glass of plain water, stay upright for at least 60 minutes, and don’t eat or drink anything else during that time. If your GERD is severe or you have trouble swallowing, your doctor may recommend an alternative like denosumab or zoledronic acid.
Why do I need to stay upright for 60 minutes?
Bisphosphonates can irritate the esophagus if they linger. Staying upright helps the pill move quickly into your stomach. Research shows that 30 minutes isn’t enough for everyone - especially older adults or those with slow esophageal movement. The FDA updated its label in 2023 to require 60 minutes to reduce injury risk.
What happens if I forget and lie down after taking my pill?
If you lie down accidentally, sit up immediately and drink a full glass of water. Don’t take another dose. Missing one dose isn’t dangerous - but repeated mistakes can cause esophagitis or ulcers. If you often forget to stay upright, talk to your doctor about switching to an injectable option.
Are there safer alternatives to oral bisphosphonates?
Yes. Denosumab (Prolia) is a monthly injection with no esophageal risk. Zoledronic acid (Reclast) is an annual IV infusion. Both avoid the esophagus entirely. Teriparatide and romosozumab are also alternatives but are much more expensive and have other side effects. Your doctor can help you weigh cost, convenience, and risk.
Can bisphosphonates cause esophageal cancer?
Early studies raised concerns, but recent data from the NIH’s ongoing Bisphosphonate Safety Study shows no significant increase in esophageal cancer risk through five years of follow-up. The FDA still lists it as a potential risk due to conflicting past data, but current evidence suggests the risk is very low - if it exists at all - when the drugs are used properly.
Should I stop taking bisphosphonates if I get heartburn?
Not necessarily. Mild heartburn can be caused by improper dosing. Try following the 60-minute upright rule with plain water. If the heartburn continues, talk to your doctor. They may adjust your medication, test for GERD severity, or switch you to a safer option. Never stop a bone medication without medical advice - sudden discontinuation can increase fracture risk.






Comments
Javier Rain
I took Fosamax for three years and thought my heartburn was just stress-turns out I was lying down after taking it. Once I started the 60-minute rule with plain water? Poof. Gone. No more burning. This post saved my esophagus. Seriously, if you’re on these meds and have reflux, DO NOT skip the upright time.
Laurie Sala
Wait-so you’re telling me I’ve been doing it WRONG this whole time?!?!? I take it right before bed because I’m lazy-and now I’m terrified I’ve been slowly burning a hole in my throat???!!! I need to go check my last endoscopy report… I’m sweating just thinking about it!!!
Lisa Detanna
As someone who grew up in a culture where meals are followed by naps, this hit hard. My abuela always said, ‘After eating, rest.’ But now I know-resting after bisphosphonates is dangerous. I’ve started telling my elderly relatives about this. We need better education-not just for Americans, but globally. This isn’t just medical advice, it’s cultural adaptation.
Demi-Louise Brown
Proper medication administration is critical in geriatric populations. The 60-minute upright requirement is not arbitrary; it is grounded in pharmacokinetic data demonstrating delayed gastric emptying in older adults. Failure to adhere results in localized drug exposure and mucosal injury. Clinical guidelines from the American College of Rheumatology reinforce this protocol.
Matthew Mahar
bro i took mine with orange juice once because i was in a rush… i swear i felt like my chest was on fire for 3 hours… i thought i was having a heart attack… turned out it was just my esophagus screaming at me for being dumb… dont be me
Casper van Hoof
The ethical dilemma presented here is not merely pharmacological but existential: when does the pursuit of skeletal integrity justify the potential degradation of gastrointestinal autonomy? The pharmaceutical industry promotes these agents as cost-effective, yet the burden of compliance falls disproportionately on the aging patient, who is often cognitively and physically compromised. Is this truly patient-centered care?
Richard Wöhrl
Just want to add: if you're on PPIs and still getting heartburn after taking bisphosphonates, it's not the acid-it's the pill getting stuck. PPIs reduce stomach acid, but they don't speed up esophageal transit. That's why staying upright matters even more. Also, if you're over 70, your esophagus moves slower. That 60-minute rule? It's not a suggestion-it's your body's last line of defense. I've seen patients end up in the ER because they thought '30 minutes was fine.' Don't be one of them.
Pramod Kumar
In India, many elders take these pills with tea or milk thinking it’s gentler. Big mistake. I told my uncle-he switched to plain water and standing for an hour. No more burning. He even started doing it in the garden, sipping water, watching the sunrise. Now he calls it his ‘bone meditation.’ Sometimes the fix isn’t medicine-it’s ritual.
Lisa Lee
U.S. doctors are so obsessed with pills they forget we have bodies. Why not just inject it? Why make old people do gymnastics just to take a pill? Canada doesn’t make us jump through these hoops. We have better systems. This is why I hate American healthcare.
Charmaine Barcelon
You people are so naive. You think following rules will save you? My cousin took it perfectly-upright, water, no food-and still got ulcers. It’s the drug. It’s toxic. Stop pretending it’s just about how you take it. Your doctor is just selling you a false sense of control.
Karla Morales
OMG I JUST REALIZED I’VE BEEN TAKING MINE AT NIGHT 😭😭😭 I’M SO SCARED RIGHT NOW. I NEED TO CALL MY DOCTOR. I’M GOING TO DIE FROM A BURNED ESOPHAGUS. 😭🩸💔
John Mackaill
My father was on alendronate for five years. He never had symptoms, but his endoscopy showed silent damage. That’s the scary part-it doesn’t always hurt until it’s too late. If you’re on these long-term, get checked-even if you feel fine.
Adrian Rios
I’ve been managing osteoporosis for over a decade, and I’ve tried every single option. Oral bisphosphonates? They’re cheap, sure-but the lifestyle toll is real. You become a slave to timing, water, posture. I switched to Reclast last year. One IV a year. No rules. No stress. No fear of lying down after lunch. The cost is high, but my peace of mind? Priceless. And honestly, if you’re taking this seriously, you’re already doing better than most people who just swallow pills and hope for the best.
Brandy Walley
Everyone’s acting like this is some groundbreaking advice. I’ve been taking Fosamax for 8 years and never had an issue. You’re all overreacting. Maybe you just have weak stomachs. Stop blaming the drug. Blame your diet. Or your laziness. Or your anxiety.
shreyas yashas
my grandma took bisphosphonates and never followed any rules. she lived to 94. maybe the real danger is worrying too much?