OIC Treatment Decision Tool
Personalized OIC Treatment Assistant
This tool helps determine the most appropriate treatment options for opioid-induced constipation based on your specific situation. Your inputs will generate personalized recommendations for managing OIC.
Your Treatment Recommendations
Select your options and click "Get My Treatment Plan" to see personalized recommendations.
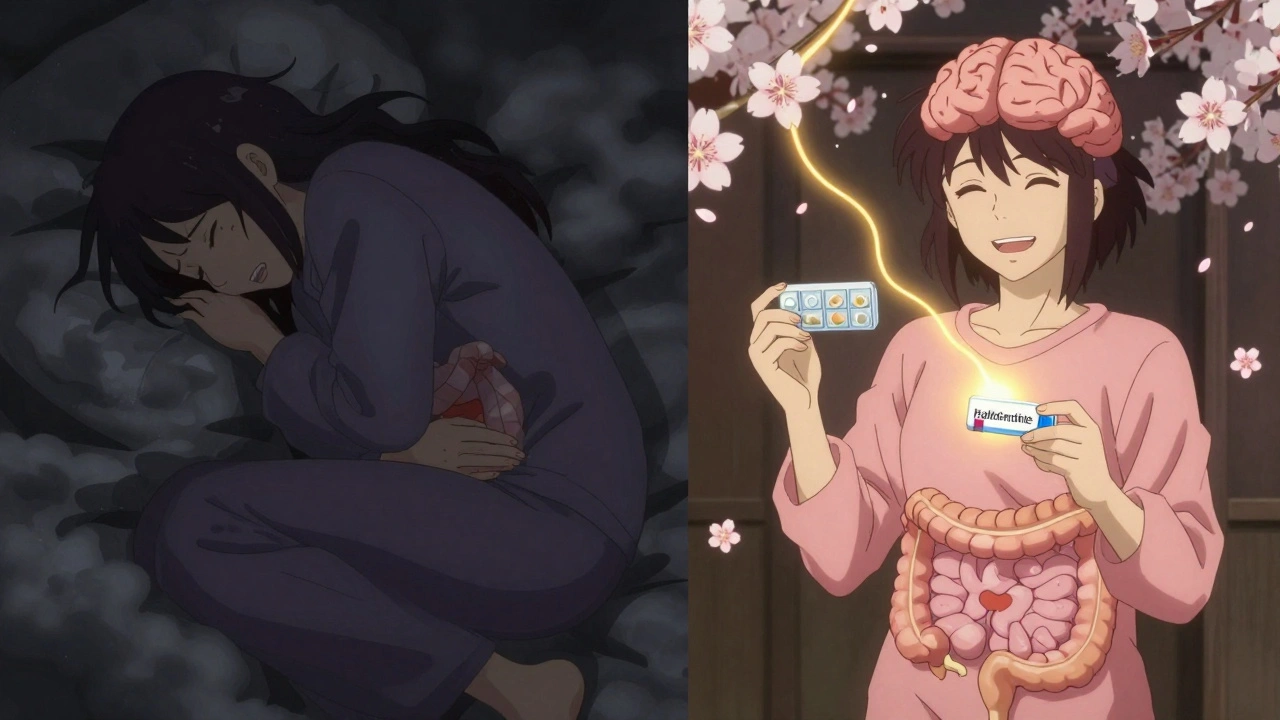
When you start taking opioids for chronic pain, you’re told about the risks-drowsiness, nausea, addiction. But one of the most common and persistent side effects is rarely mentioned until it’s already wrecking your life: opioid-induced constipation. It’s not just a minor inconvenience. For 40 to 60% of people on long-term opioids, it’s a daily battle with bloating, straining, and the feeling that your bowels have shut down for good. And unlike other side effects that fade over time, OIC doesn’t get better. It only gets worse if you ignore it.
Why Opioids Cause Constipation
Opioids don’t just block pain signals in your brain. They also latch onto receptors in your gut, specifically the μ-opioid receptors in the intestinal wall. This slows down the natural muscle contractions that push food and waste through your digestive system. Your stomach empties slower. Your colon absorbs more water from stool. And the muscle around your anus tightens, making it harder to push anything out. The result? Hard, dry stools. A constant feeling of incomplete evacuation. Straining that lasts longer than a few minutes. Sometimes, you feel like you need to go-but nothing comes. This isn’t normal constipation. It’s not caused by eating too little fiber or drinking too little water. It’s a direct effect of the drug itself. And it doesn’t go away just because you’ve been on opioids for months.Prevention Starts on Day One
The biggest mistake people make? Waiting until they’re constipated before doing anything. By then, the problem is already entrenched. Experts agree: if you’re starting opioids, you should start a laxative at the same time. Not tomorrow. Not next week. Today. Studies show that proactive laxative use prevents 60 to 70% of severe OIC cases. That’s not a guess. That’s what doctors at Johns Hopkins and Mayo Clinic have seen in real patients. The key is consistency. Don’t wait for symptoms. Don’t skip doses because you feel fine. Your gut is already slowing down-even if you don’t notice it yet.First-Line Treatment: Laxatives That Actually Work
Not all laxatives are created equal when it comes to OIC. Over-the-counter options like senna or bisacodyl (stimulant laxatives) and polyethylene glycol (an osmotic laxative) are the most effective starting points. Polyethylene glycol, sold as MiraLAX, pulls water into the colon to soften stool without irritating the gut lining. It’s gentle, safe for long-term use, and doesn’t cause dependency. Stool softeners like docusate? They’re popular, but they don’t do much for OIC. Same with fiber supplements. Fiber can make things worse if you’re not drinking enough water, and opioids already slow everything down too much for fiber to help. Enemas and suppositories can give quick relief in emergencies, but they’re not a long-term solution. You can’t live on enemas forever. And if you’re already relying on them regularly, it’s a sign your treatment plan needs upgrading.When Laxatives Aren’t Enough: PAMORAs
If you’ve been on laxatives for weeks and still feel backed up, it’s time to talk about PAMORAs-peripherally acting μ-opioid receptor antagonists. These are prescription drugs designed to block opioids’ effects in your gut without touching their pain-relieving power in your brain. There are four main ones:- Methylnaltrexone (Relistor®): Given as a subcutaneous injection. Works in under 30 minutes. Used mostly in palliative care, but effective for anyone who needs fast relief.
- Naldemedine (Movantik®): A daily pill. Approved for cancer patients and those on chronic opioids. Studies show it also reduces opioid-induced nausea.
- Naloxegol (Movantik®): Another daily pill. Works similarly to naldemedine but with slightly different side effects.
- Lubiprostone (Amitiza®): A chloride channel activator. Increases fluid secretion in the gut. FDA-approved for women, but works in men too.

The Hidden Risks
PAMORAs aren’t risk-free. All of them carry a warning: they can cause gastrointestinal perforation. That’s a tear in the intestinal wall. It’s rare-but it’s serious, sometimes deadly. That’s why they’re not for everyone. Avoid PAMORAs if you have:- A known or suspected bowel obstruction
- Recent abdominal surgery
- Active inflammatory bowel disease (Crohn’s, ulcerative colitis)
- Severe abdominal scarring
Cost and Access Are Major Barriers
Here’s the hard truth: even if PAMORAs work, you might not be able to get them. A single month’s supply of naldemedine or methylnaltrexone can cost $500 to $900 without insurance. Most insurance plans require prior authorization. Medicare Part D plans require it 41% of the time. Commercial insurers often force you to try and fail on cheaper laxatives first-called step therapy. A 2023 survey found that 57% of patients stopped taking PAMORAs within six months because of cost or lack of results. That’s not just a financial problem. It’s a healthcare failure. When patients can’t afford treatment, they suffer in silence. They stop taking their pain meds. They end up in the ER with fecal impaction. The American Society of Gastroenterology estimates that poor OIC management costs the U.S. healthcare system $2.3 billion every year.What Works Best for Different People
There’s no one-size-fits-all. Your treatment should match your life.- Cancer patients on regular opioids: Naldemedine is recommended by ASCO guidelines because it helps with both constipation and nausea.
- Patients needing fast relief: Methylnaltrexone injections work in minutes. A new once-weekly version is now available, making it easier to manage.
- People who hate injections: Naldemedine and naloxegol are pills. Daily, but no needles.
- Women with OIC: Lubiprostone is FDA-approved for women, but works well in men too. Just watch for nausea.





Comments
Aman deep
Man, this post hit home. I’ve been on oxycodone for 3 years after my back surgery, and no one ever warned me about the constipation. I thought I was just eating wrong. Turns out, my gut was basically on vacation. Started MiraLAX on my doc’s advice-life saver. No more screaming at the toilet at 3 a.m. Just wish someone had told me this before I lost 12 pounds from not eating because I was too bloated to even look at food.
Sarah Clifford
So basically opioids turn your colon into a brick factory and the docs just shrug? Yeah right. I bet the pharma companies love this. They make billions off pain meds and then sell you another $800 pill to fix what they broke. Classic.
Ben Greening
Interesting breakdown. The BFI tool is underutilized in primary care. I’ve seen patients endure months of discomfort before anyone even measures severity. Objective metrics matter-especially when symptoms are subjective and dismissed as ‘just part of it.’
Lisa Stringfellow
Wow, another ‘here’s how to fix your body’ guide from someone who clearly doesn’t live in the real world. You think telling someone on opioids to just take a laxative is enough? Have you ever tried to swallow a pill when you’re too dizzy to stand? Or paid $900 for a pill that your insurance denies because you didn’t ‘fail’ three cheaper ones first? This isn’t medicine. It’s a corporate checklist.
Regan Mears
Lisa, I hear you-this system is broken. But blaming the patient for not ‘trying hard enough’ doesn’t help. The real failure is that doctors don’t get trained on OIC until it’s an emergency. I’ve seen patients get admitted for fecal impaction because their PCP didn’t know to prescribe MiraLAX on day one. It’s not laziness-it’s ignorance. And that’s fixable.
Stephanie Maillet
There’s a deeper philosophical layer here: we treat pain as the only valid symptom, while ignoring the body’s other systems as if they’re secondary. But the gut is the second brain-when it’s silenced, the whole self is silenced. Is our medical paradigm so narrowly focused on ‘pain control’ that we’ve forgotten the body is an interconnected whole? Or are we just too comfortable with pharmaceutical band-aids?
Nikki Smellie
Have you all noticed that every single PAMORA is made by a big pharma company with a history of hiding side effects? And now they’re selling us a ‘magic pill’ that ‘doesn’t affect the brain’? Please. If it’s blocking opioid receptors, how is it NOT affecting the brain? They’re lying. This is a controlled release of suffering-so you keep taking the pain meds, and they keep making money. I’ve seen the documents. It’s not coincidence.
Rebecca Dong
So what’s the REAL reason they don’t warn people? Because if you knew your bowels were going to turn to concrete, you’d say NO to opioids. And then the opioid industry collapses. This is a deliberate cover-up. The FDA knew. The AMA knew. They just didn’t care enough to tell you. You’re not sick-you’re being exploited.
Sylvia Frenzel
My husband’s on methadone. We tried everything. Laxatives? Used up. Enemas? He cried. Then we got naldemedine. First day, he had a normal bowel movement. No pain. No panic. Just… relief. It’s expensive. Insurance fought us. But we appealed. And now he can sleep through the night without worrying he’ll explode. This isn’t a luxury. It’s dignity.