Getting your medication isn’t just about picking it up at the pharmacy. For millions of people, the real hurdle comes when they see the price tag. Medication adherence-taking your drugs exactly as prescribed-isn’t just a medical term. It’s a matter of life and death. And one of the biggest reasons people skip doses, split pills, or skip refills altogether? Cost.
In 2021, nearly 1 in 12 American adults under 65 didn’t fill a prescription because they couldn’t afford it. That’s 8.2% of people managing chronic conditions like high blood pressure, diabetes, or heart disease. And it’s not just the uninsured. Even people with Medicare or private insurance are struggling. One 62-year-old woman in a Kaiser survey said she pays $350 a month for her meds after insurance. That’s more than her monthly grocery budget. So she chooses: pills or food?
The numbers don’t lie. A 2022 analysis of 71 studies found that 84% showed a direct link between higher out-of-pocket costs and worse adherence. When a copay jumps from $10 to $50, adherence drops by 15-20%. For people with heart disease, the effect is even sharper. Skip a dose of your blood pressure pill? Your risk of stroke or heart attack goes up. Don’t take your insulin? Your blood sugar spirals. And it’s not just health-it’s money. Non-adherence causes an estimated $100-$300 billion in avoidable hospital visits, ER trips, and complications every year.
Why Are Medications So Expensive?
It’s not just about the pill in the bottle. The cost comes from layers: high list prices, insurance formularies that push you toward pricier brands, deductibles you haven’t met yet, and coinsurance that takes 20-40% of the cost. Even with insurance, you might pay $800 a month for insulin. That’s not a typo. A 2016 study found insulin list prices rose 368% between 2007 and 2017-even though manufacturing costs barely changed.
Pharmacies don’t set these prices. Drugmakers do. And while generics have helped-1,123 were approved in 2022 alone-many life-saving drugs still have no cheap alternatives. Patients often don’t know their drug is on a high-tier formulary until they’re at the counter. One survey found 41% of patients experienced "sticker shock"-the moment their expected $30 pill turns out to be $150.
Low-income patients, especially women and people of color, are hit hardest. Many say they skip meals, delay rent, or skip other essential care just to afford their meds. The CDC found non-adherence rates are over three times higher for people earning under $25,000 a year compared to those earning over $75,000.
How Cost Affects Your Health
Skipping doses doesn’t mean "I’ll take it tomorrow." It means your body doesn’t get the steady dose it needs to stay stable. For blood pressure meds, missing even one dose can spike your numbers. For antidepressants, it can trigger a relapse. For antibiotics, it can lead to resistant infections.
The American Heart Association estimates that 125,000 Americans die each year because they didn’t take their meds as directed. That’s more than traffic accidents or gun violence. And it’s preventable.
People don’t skip meds because they’re careless. They do it because they’re forced to. One Reddit user shared how they split their 100mg pill in half to make it last longer. Another said they waited three weeks to refill their inhaler because they were waiting for their next paycheck. These aren’t rare stories. They’re everyday realities.
What You Can Do Right Now
You don’t have to choose between your health and your rent. Here’s what works-based on real patient experiences and proven programs.
- Ask your doctor about alternatives. Not every drug on the market is equally priced. Your doctor can check if there’s a generic, a lower-tier brand, or a similar drug covered better by your plan. The American Medical Association says this is the #1 thing providers should do.
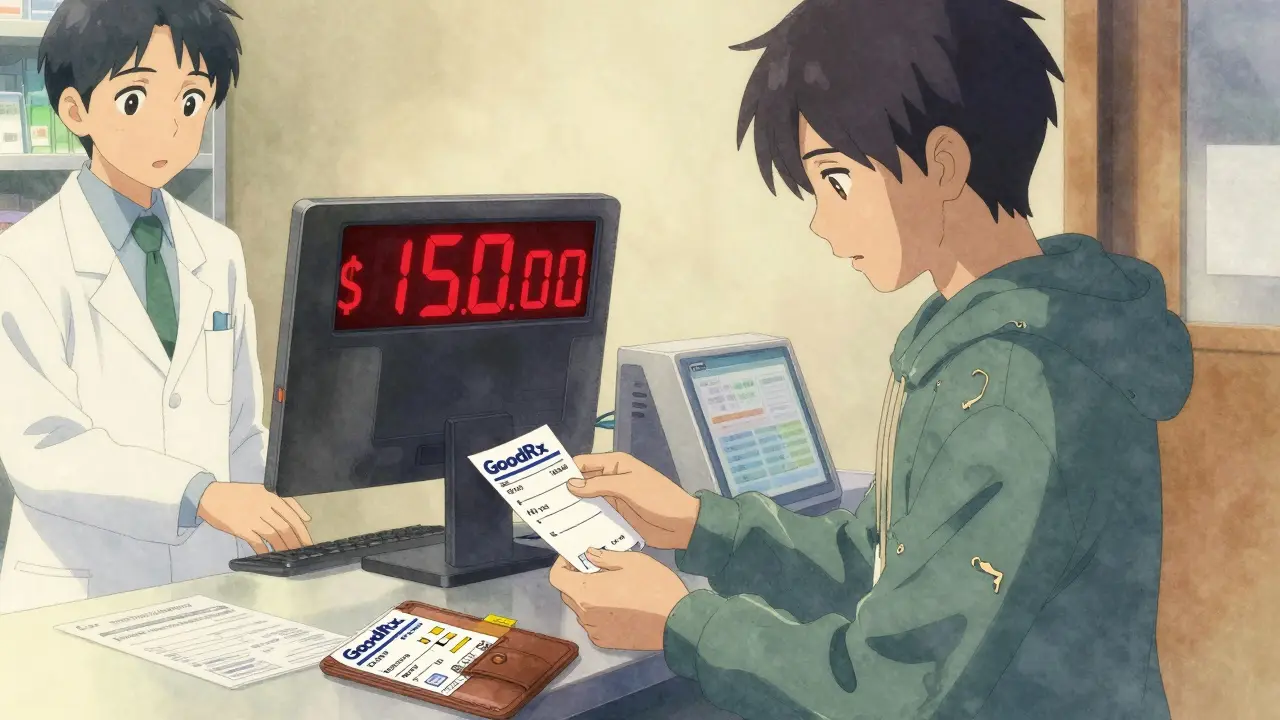
- Use GoodRx or SingleCare. These free apps compare prices at nearby pharmacies. One user saved 78% on their cholesterol med-paying $12 instead of $55. Over 35 million Americans use them monthly.
- Ask for a 90-day supply. Many insurers charge less per pill for a three-month supply. Mail-order pharmacies often offer this too. You’ll save 20-30% and reduce how often you have to pay.
- Check for patient assistance programs. Pharmaceutical companies run these for people with low income. In 2022, they helped 1.8 million people. Eligibility? Usually under 400% of the federal poverty level-that’s $55,520 for one person in 2023. Programs like Patient Services Inc. and the Partnership for Prescription Assistance can help you apply.
- Ask for samples. Doctors still have free samples. Don’t be shy. One patient said her insulin cost dropped from $500 to $25 after getting on a manufacturer’s program.
- Use Medicare’s Extra Help program. If you’re on Medicare and have limited income, this program can cover up to $5,000 a year in drug costs. Apply at SSA.gov.
What’s Changing in 2025?
The Inflation Reduction Act brought real changes to Medicare Part D. Starting in 2025, out-of-pocket drug costs for seniors will be capped at $2,000 a year. The infamous "donut hole" is gone. And you’ll be able to pay for high-cost meds in monthly installments instead of one big bill.
Hospitals and insurers are also rolling out real-time benefit tools (RTBTs). These show your doctor the exact price of a drug before they write the prescription. In 2024, 78% of large health systems will have them. That means less sticker shock.
But experts warn: these fixes aren’t enough. The Congressional Budget Office predicts drug spending will hit $1.1 trillion by 2031. Without deeper pricing reforms, 1 in 5 Americans will still skip meds because they can’t afford them-even with insurance.

When You’re Ready to Talk to Your Doctor
Saying "I can’t afford this" is hard. But your doctor isn’t there to judge. They’re there to help you stay alive. Try these phrases:
- "I’m having trouble paying for this. Is there a cheaper option?"
- "Can we check if this drug is on my insurance’s lowest tier?"
- "I’ve been skipping doses because of the cost. Can we find a solution?"
Doctors who talk about cost with patients are 65% more likely to have patients who stick with their meds. That’s a huge win.
Final Thoughts
Medication adherence isn’t about willpower. It’s about access. You shouldn’t have to choose between your health and your rent. The system is broken-but you’re not powerless. Use the tools. Ask the questions. Apply for help. Millions have done it before you. And it works.
If you’re taking meds for a chronic condition, your health depends on consistency. Don’t let cost steal that from you. Start today. Call your pharmacy. Check GoodRx. Ask your doctor. You’ve got options.
Why do people skip their medications because of cost?
People skip doses, split pills, or delay refills because out-of-pocket costs are too high-even with insurance. Copays, deductibles, and tiered formularies can make life-saving drugs cost hundreds of dollars a month. Many choose between paying for meds and buying food, rent, or utilities. Studies show 8.2% of adults under 65 and 14.4% of Medicare beneficiaries have skipped meds due to cost.
Can I get my prescriptions for free?
You may qualify for free or low-cost meds through patient assistance programs run by drug manufacturers. These are available to people with incomes under 400% of the federal poverty level ($55,520 for one person in 2023). Programs like Patient Services Inc. and the Partnership for Prescription Assistance help you apply. Some drugs also offer free samples from your doctor.
Does Medicare cover all my prescription costs?
No. Medicare Part D has gaps like deductibles and coinsurance. Many seniors still pay hundreds a month. But starting in 2025, the out-of-pocket cap for Medicare Part D will be $2,000 a year, and the "donut hole" will be eliminated. Low-income beneficiaries can also apply for Extra Help, which covers up to $5,000 in annual drug costs.
How can I find the cheapest pharmacy for my meds?
Use free apps like GoodRx or SingleCare. They show you the lowest cash price at nearby pharmacies-often 50-80% cheaper than your insurance copay. Prices vary wildly between stores, even for the same drug. One user saved $43 on a blood pressure pill just by switching pharmacies.
Should I ask my doctor for a cheaper alternative?
Yes. Your doctor can check if your drug is on your insurance’s lowest tier, switch you to a generic, or prescribe a similar but cheaper medication. The American Medical Association says checking formulary alignment before prescribing is one of the most effective ways to improve adherence. Don’t be embarrassed-cost conversations are now routine for 65% of doctors.
What happens if I stop taking my medication because of cost?
Stopping meds can lead to serious health problems. Skipping blood pressure pills raises stroke risk. Missing insulin can cause diabetic emergencies. For heart disease, non-adherence is linked to 125,000 deaths a year in the U.S. It also leads to more ER visits and hospital stays, which cost the system $100-$300 billion annually. The short-term savings aren’t worth the long-term risk.







Comments
Monte Pareek
Look I get it you think this is about willpower but it's not it's about capitalism eating people alive
I work two jobs and still split my insulin pills because $400 a month is more than my rent
My doctor told me to use GoodRx but the closest pharmacy that has the price is 40 miles away and I don't have a car
They give you pamphlets instead of solutions
And don't even get me started on how the pharma reps show up at clinics pushing the expensive stuff because they get bonuses for it
They don't care if you live or die they care if the stock goes up
I've seen people cry in the pharmacy line because their copay went up $80 and they had to choose between meds and their kid's school supplies
And yeah I know about patient assistance programs but the paperwork is a nightmare and you need a lawyer just to fill out the forms
Meanwhile the CEOs get bonuses while people die
This isn't a health crisis it's a moral failure
Kelly Mulder
Let me be perfectly clear: the notion that patients are somehow "responsible" for navigating a system designed to extract wealth under the guise of healthcare is not only naive-it is grotesque.
The pharmaceutical industry operates as a legalized cartel, leveraging patent monopolies and regulatory capture to inflate prices beyond any rational economic model.
Insulin, a 100-year-old molecule, should cost $2 per vial-not $300. The fact that we tolerate this is not a market failure-it is a societal collapse.
And yet, we are told to "ask your doctor" or "use GoodRx" as if these are equitable solutions rather than Band-Aids on a hemorrhage.
There is no moral high ground here. Only complicity.
mark shortus
OMG I CRIED WHEN I READ THIS
I just got diagnosed with Type 2 and my first script was $700
I sat in my car for an hour just staring at the receipt
I thought about not filling it
My mom had to send me $200 just so I could get through the week
And then I saw a commercial for some new diabetes drug that costs $1,200 a month and it’s like... what the actual f***
Why are we letting this happen
I’m not lazy I’m not stupid I’m just broke
And I’m not alone
Someone needs to burn this system down
Chris Clark
Been there. Used to be a nurse in rural Ohio.
Old lady came in with her pill bottle-half the pills were gone.
Asked why.
She said "I take one every other day. The other one’s for my husband. He’s got high blood pressure too. We split the bottle. We don’t tell the doctor. We don’t want them to think we’re crazy."
That’s the reality. People are doing triage with their lives.
And yeah GoodRx helps sometimes but not if you’re on Medicaid and they don’t honor it.
Or if you’re undocumented and scared to even ask.
Or if you’re 72 and can’t figure out how to use an app.
We need systemic change. Not tips.
William Storrs
You’re not alone. I know how scary it feels to look at that price and wonder if you can keep going.
But here’s the thing-you’ve already taken the hardest step: you’re looking for help.
That’s courage.
Now take the next one: call your pharmacy. Ask for samples. Check Patient Services Inc. It takes 20 minutes. Maybe less.
I’ve seen people go from skipping meds to stable, healthy, back to work-all because they asked one question.
You don’t have to fix everything today.
Just do one thing.
One thing can change everything.
Guillaume VanderEst
Man, I’m from Montreal and we got universal coverage here, but I’ve seen friends cross the border just to buy insulin in the U.S. because it’s cheaper than here after taxes and co-pays.
That’s messed up.
And yeah, I’ve seen people in my town skip meals to afford their meds.
It’s not just a U.S. problem-it’s a global shame.
But I guess we’re all just supposed to smile and say "thanks for the pamphlet" while our neighbors die.
Henry Marcus
THIS IS A DEEP STATE OPERATION.
Big Pharma, the FDA, the AMA-they’re all in cahoots.
They’re not letting generics in because they want you dependent.
They’re using the "donut hole" and "formularies" to keep you confused and powerless.
And don’t think the government doesn’t know-Congress gets millions in pharma donations every year.
That $2,000 cap in 2025? A distraction.
They’ll raise premiums next year.
They’ll add new fees.
They’ll invent new tiers.
This isn’t reform-it’s theater.
And the real solution? Nationalize drug manufacturing.
Right now.
Carolyn Benson
It’s not about access.
It’s about the metaphysical weight of being forced to choose between your body and your dignity.
The pill is not just a chemical compound.
It’s a symbol of a society that commodifies survival.
When you split a pill, you’re not just rationing medicine-you’re rationing your right to exist without shame.
And yet, we call this "personal responsibility".
How convenient.
The system doesn’t fail you.
It was designed to do exactly this.