When you pick up a prescription, you might not realize there are two very different kinds of medications on the shelf - and they can cost you dramatically different amounts. One is made by a single company with no competitors. The other is made by many, often at a fraction of the price. Understanding the difference between single-source and multi-source drugs isn’t just about pharmacy jargon - it’s about saving money, avoiding confusion, and making sure your treatment works as expected.
What exactly is a single-source drug?
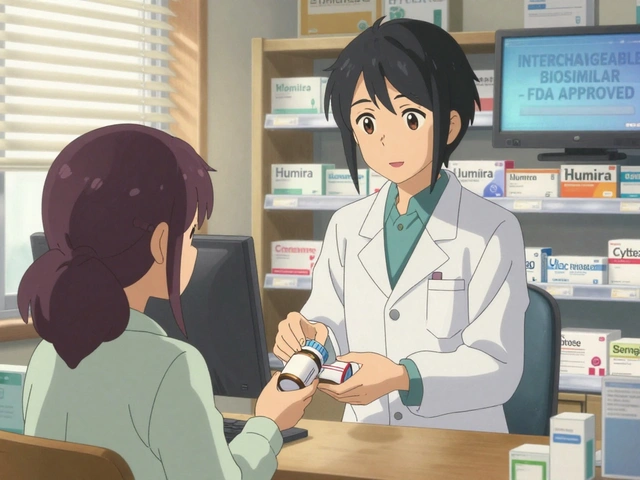
A single-source drug is a medication that only one company is allowed to make. Usually, this means it’s still under patent protection or has some kind of market exclusivity. Think of it like the original version - the one you see advertised on TV. Examples include Humira (for autoimmune diseases), Lantus (for diabetes), and many newer cancer drugs.Because no one else can make it yet, the manufacturer sets the price. There’s no competition. That’s why these drugs often cost hundreds or even thousands of dollars a month. In 2023, the average monthly cost for a single-source drug was around $587, according to a Kaiser Family Foundation survey. And because there’s no generic version, your insurance may force you to pay a high copay - or deny coverage altogether unless you try cheaper alternatives first.
Even worse, some single-source drugs have "authorized generics" - where the brand company itself releases a cheaper version. But even then, the price doesn’t always drop much. That’s because the company controls both versions. It’s not real competition. It’s just a different label.
What makes a drug multi-source?
A multi-source drug is one that has at least one generic version approved by the FDA. Once a patent expires, other companies can step in and make the same medicine - using the same active ingredient, same strength, same way of taking it. These are called generics. But there’s also something called a "multi-source brand" - that’s when the original brand is still sold, but generics are available too.Here’s the key: every generic must prove it works the same as the brand. The FDA requires it to be bioequivalent - meaning your body absorbs it at the same rate and in the same amount. The acceptable range is 80% to 125% of the brand’s performance. That’s not a loophole - it’s science.
Multi-source drugs make up about 90% of all prescriptions filled in the U.S., but they only account for 23% of total drug spending. That’s because generics cost way less. The average monthly price? Around $132. That’s more than four times cheaper than single-source drugs.
Why do generics cost so much less?
It’s simple: no marketing, no patents, no research costs. Generic manufacturers don’t have to spend millions proving the drug works - that’s already been done. They just need to prove their version behaves the same way in your body.Pharmacies and insurers use something called Maximum Allowable Cost (MAC) to set what they’ll pay for a generic. MAC prices are usually 50% to 60% lower than the brand’s average wholesale price. Insurers use this to push you toward generics - and they’re successful. In 2022, Medicare Part D beneficiaries filled 82% of their prescriptions with generics or multi-source drugs, up from 73% in 2017.
But here’s the twist: even though generics are cheaper, your out-of-pocket cost doesn’t always reflect that. Some insurance plans still charge you a high copay for a generic if it’s on a higher tier. Or worse - they switch you to a different generic manufacturer without telling you. That’s more common than you think. A 2022 report found 63% of patients on multi-source drugs had their generic switched at least once in a year.

Do generics work the same as brand-name drugs?
The FDA says yes. All approved generics must meet the same strict standards. They contain the same active ingredient. They’re made in the same type of facilities. They’re tested for safety and effectiveness.But patient experiences tell a different story. On Drugs.com, multi-source drugs have an average rating of 4.2 out of 5.0. Single-source drugs? 4.5. That gap might seem small, but when you’re dealing with chronic conditions like epilepsy, thyroid disease, or depression, even small differences can feel big.
Some patients report feeling different when switching between generic manufacturers. One person might get a tablet made by Teva, then get a pill from Mylan the next month. Even though both are FDA-approved, the fillers, coatings, or manufacturing processes can vary slightly. For most people, this doesn’t matter. But for those with narrow therapeutic index drugs - like warfarin, lithium, or levothyroxine - even tiny changes can affect how the medicine works.
If you notice your symptoms changing after a switch, talk to your pharmacist. Ask if the manufacturer changed. If you’re worried, ask your doctor to write "dispense as written" or "no substitutions" on your prescription.
How does insurance treat these drugs differently?
Your insurance plan doesn’t treat single-source and multi-source drugs the same way. That’s by design.Single-source drugs are usually on Tier 3 or Tier 4 of your formulary - meaning higher copays, or even prior authorization. You might have to try a cheaper generic first before your plan will cover the brand. This is called "step therapy." It’s common with drugs for arthritis, high cholesterol, or mental health.
Multi-source drugs? They’re usually on Tier 1 - the lowest cost tier. Your copay might be $5 or $10. Many insurers will even refuse to cover the brand-name version unless you’ve tried and failed with generics.
But here’s something patients rarely know: insurance companies and pharmacy benefit managers (PBMs) often get rebates from drugmakers. For single-source drugs, those rebates can be huge - and they’re tied directly to the list price. That means if the drug’s price goes up, the rebate goes up too. But guess what? Your copay doesn’t go down. You’re still paying the full list price until your deductible is met. The savings go to the insurer, not you.
For multi-source drugs, the rebate system works differently. Because there are many manufacturers competing, the price doesn’t rise as fast. And even when rebates increase, the list price doesn’t always follow. That’s why net prices for generics tend to fall over time.
What should you do as a patient?
You don’t need to be a pharmacy expert to make smarter choices. Here’s what you can do right now:- Ask if there’s a generic - even if your doctor didn’t mention it. Say: "Is there a generic version of this?"
- Check your formulary - log into your insurer’s website and look up your drug. See what tier it’s on and what the copay is.
- Ask your pharmacist - every time you pick up a prescription, ask: "Did the manufacturer change?"
- Use the FDA’s Orange Book - it lists which generics are approved and what their therapeutic equivalence code is. Look for "A" codes - those mean they’re interchangeable.
- Don’t assume brand = better - for 9 out of 10 drugs, the generic works just as well.
- Speak up if something feels off - if your energy drops, your symptoms return, or you get new side effects after a switch, tell your doctor. It’s not "in your head."
The FDA says generics are safe and effective. But real-world experience shows that for some people, consistency matters. If you’ve found a generic that works for you, stick with it. Ask your pharmacist to fill it with the same manufacturer every time - if they can.
What’s changing in 2025?
The FDA is pushing to approve generics faster. Under the new Generic Drug User Fee Amendments (GDUFA III), approval times are dropping to 10 months by 2025. That means more single-source drugs will become multi-source sooner.Take Humira - it was a single-source drug for 14 years. Now, 10+ generic versions are on the market. Prices are already falling. More drugs like it - for psoriasis, Crohn’s, rheumatoid arthritis - will follow.
At the same time, drugmakers are using "authorized generics" and "product hopping" - launching a slightly changed version right before the patent expires to delay generics. It’s legal. It’s frustrating. But you can still fight back by asking for the original generic, not the new "improved" brand.
Bottom line: You have more power than you think
Most people assume they have no control over drug costs. But you do. You can ask questions. You can request generics. You can track your pharmacy’s manufacturer changes. You can tell your doctor if something doesn’t feel right.Single-source drugs have their place - especially for new, complex treatments. But for the vast majority of medications, multi-source options are just as good and far cheaper. You’re not taking a risk by choosing a generic. You’re making a smart, evidence-based decision.
And if your insurance tries to force you into a brand you can’t afford? Push back. Ask for a formulary exception. Call your plan’s member services. You’re not alone. Millions of people have been there - and many of them saved hundreds of dollars a month by asking the right questions.
Are generic drugs as safe as brand-name drugs?
Yes. The FDA requires generic drugs to have the same active ingredient, strength, dosage form, and route of administration as the brand. They must also meet the same strict manufacturing standards. Every generic is tested for bioequivalence - meaning your body absorbs it the same way. There’s no difference in safety.
Why does my generic look different every time I refill?
Because different companies make generics, and each one uses different colors, shapes, or fillers. The active ingredient is the same, but the inactive ingredients can vary. That’s why the pill might look different. It doesn’t mean it’s less effective. But if you notice changes in how you feel after a switch, tell your pharmacist and doctor.
Can my insurance force me to switch to a generic?
Yes. Most insurance plans require you to try the generic version first before covering the brand-name drug. This is called step therapy. If the generic doesn’t work for you, your doctor can request an exception. You’ll need a letter explaining why the brand is necessary.
What’s the difference between a generic and a single-source generic?
A regular generic is made by a company other than the brand. A "single-source generic" means only one company has the right to make the generic - usually because they got exclusive rights from the brand. These aren’t always cheaper than the brand, because there’s no competition. They’re a loophole in the system.
How do I find out if my drug is single-source or multi-source?
Check the FDA’s Orange Book online - it lists all approved drugs and whether generics are available. You can also ask your pharmacist. Or call your insurance plan and ask if your drug has generic alternatives. If it does, it’s multi-source. If not, it’s single-source.
If you’re on a long-term medication, take five minutes today to check your prescription. Ask your pharmacist if a cheaper generic exists. You might be surprised how much you can save - without sacrificing quality.




Comments
Gerald Cheruiyot
Just took my levothyroxine switch last month. Felt like a zombie for two weeks. Turned out the new batch had a different filler. My pharmacist didn't tell me. Now I ask every time. No more guessing games. Life's too short for mysterious fatigue.
Also, why do we still call them 'generics'? Sounds like a discount brand of cereal. We should just call them 'equivalent meds'. Less stigma.
Michael Fessler
Let's clarify bioequivalence: FDA mandates 80–125% AUC and Cmax range for generics. That’s a 45% window-wide enough to matter for drugs with narrow therapeutic indices like warfarin or phenytoin. Not all generics are created equal in clinical practice. The FDA approves them, but real-world pharmacokinetics vary due to excipients, dissolution rates, and manufacturing tolerances. Patients on chronic therapy need consistency, not cost savings at the expense of stability.
Also, MAC pricing is a black box. PBMs negotiate rebates behind closed doors. You’re paying list price until deductible, but the rebate goes to the insurer. That’s why brand prices keep climbing. It’s not broken-it’s designed that way.
daniel lopez
THEY’RE LYING TO YOU. The FDA doesn’t test generics like they test brand names. They use ‘bioequivalence’ as a loophole. Real clinical trials? Nah. They just check blood levels in 24 healthy volunteers for 7 days. What about elderly patients? Diabetics? People with liver disease? NOBODY TESTS THAT.
And don’t get me started on the ‘authorized generics’-same company, same factory, same pill, different label. That’s price gouging with a wink. The whole system is rigged. Big Pharma owns the FDA. You think your insulin is cheaper now? It’s not. They just moved the money around.
And why do you think they push generics? So you don’t notice when your brand gets discontinued. They let the patent expire, then release their own ‘generic’ at 90% of the brand price. Genius. You’re being played.
Nosipho Mbambo
Okay, so... I read this. And I’m confused. So... generics are cheaper? But sometimes they don’t work? And insurance switches them without telling you? And the FDA says they’re fine, but people feel different? And there’s this Orange Book thing? And PBMs? And rebates? And... wait, what’s a PBM again?
Can someone just... summarize? In like, three sentences? And maybe tell me what I should do before my next refill? I just want to not feel sick and not go broke. That’s it. That’s all I ask.
Katie Magnus
Ugh. So basically, you’re saying I’m just a dumb peasant if I can’t afford Humira? Like, oh, just take the $132 generic, sweetie, it’s the same thing. But when I switched, I had a panic attack every night. My skin broke out. I cried in the shower. And my doctor said, ‘It’s all in your head.’
Newsflash: not all bodies are the same. And if your life depends on this pill, you don’t get to be ‘9 out of 10.’ You’re the 1. And now you’re being punished for needing stability.
Also, why are we still talking about this like it’s a pharmacy trivia game? This is life. Not a spreadsheet.
King Over
Generic works fine for me. No issues. Been on the same one for 5 years. Pharmacist changes it sometimes. I don’t care. Pill looks different. Tastes same. Works same. Stop overthinking it.
Also, why do people act like brand name = premium? It’s just a logo. The chemistry is identical. You’re not buying status. You’re buying medicine.
Johannah Lavin
OMG YES. I switched from brand Lantus to generic insulin and my blood sugar went wild for 3 weeks. I thought I was doing something wrong. Turns out the manufacturer changed. My endo had no idea. I had to call my pharmacy and beg for the old one. They said ‘we can’t guarantee it’ but I cried and they found it.
Don’t let anyone tell you your experience isn’t valid. If you feel different, it’s real. Ask for ‘dispense as written.’ It’s your right. And if your pharmacist rolls their eyes? Find a new one. You deserve consistency. You’re not being difficult. You’re being smart. 💪❤️
Ravinder Singh
Bro, this is gold. I’m from India, and here generics are the ONLY option. We don’t even have brand names in most villages. But guess what? People live. People thrive. My aunt has been on generic metformin for 12 years. No issues. No drama.
Yes, some people react to fillers. But that’s not the norm. The system’s flawed? Absolutely. But the answer isn’t fear-it’s awareness. Ask your pharmacist. Check the Orange Book. Know your code. A = interchangeable. B = not. Simple.
And if your insurance won’t cover your preferred generic? File a formulary exception. Most get approved. You’ve got more power than you think. Stay calm. Stay informed. 🙏
Russ Bergeman
Wait. You’re telling me that patients are actually expected to know about MAC pricing, formulary tiers, and bioequivalence ranges? That’s ridiculous. You’re blaming the patient for a broken system. The pharmacy should tell you when the manufacturer changes. The insurer should notify you before switching. The doctor should know which generics have consistent bioavailability.
But they don’t. So why are we lecturing people to ‘ask questions’? We’re not doctors. We’re not pharmacists. We’re just people trying to survive. Stop gaslighting us into self-advocacy as the solution. Fix the system. Not the patient.
Dana Oralkhan
I’ve been on the same generic for my antidepressant for 8 years. Then one month, the pill changed color and I felt like I was drowning. I didn’t know why. I thought I was relapsing. Turns out, it was a new manufacturer. I called my pharmacy. They apologized. Gave me the old one. No hassle.
So if you’re feeling off after a refill? Don’t blame yourself. Don’t panic. Just ask: ‘Is this the same maker?’
It’s not complicated. And you’re not being difficult. You’re being careful. That’s smart. Not crazy.
Jeremy Samuel
Generics? Nah man. I tried one once. Felt like my brain was wrapped in saran wrap. Took me 3 weeks to feel normal again. Now I pay full price. Worth it. Who cares if I’m broke? I’d rather be lucid than cheap.
Also, why do people say ‘FDA says it’s fine’ like that’s the end of the conversation? I don’t trust the FDA. They approved OxyContin. Need I say more?
Destiny Annamaria
Y’all are overcomplicating this. I’m a single mom. I don’t care about bioequivalence or MAC pricing. I care that my kid’s asthma inhaler doesn’t cost $600 a month. So I ask: ‘Is there a cheaper one?’ And if they say yes, I take it. And if I feel weird? I go back. Simple. Done.
Also, my pharmacist is my hero. She remembers my name. She tells me when the maker changes. I don’t need a PhD. I need a good pharmacy.
Ron and Gill Day
Wow. So you’re saying patients should be pharmacists? That’s hilarious. You think the average person knows what ‘bioequivalence’ means? Or that they have time to check the Orange Book? Or that they’re not terrified of their insurance company?
This isn’t empowerment. It’s victim-blaming wrapped in a ‘smart consumer’ bow. The real problem? Drug companies. PBMs. Congress. Not the person trying to breathe.
Stop pretending this is about education. It’s about profit. And you’re helping them.
Summer Joy
I switched to a generic for my thyroid med and I had a full-on breakdown. Literally. I screamed in the parking lot. My husband thought I was having a stroke. Turns out, the new generic had a different coating. It dissolved slower. My TSH went from 2.1 to 7.8.
I went to my doctor. She said, ‘It’s probably nothing.’ I cried. I showed her the lab results. She called the pharmacy. They said, ‘We don’t track that.’
Now I pay $150/month out of pocket for the brand. I don’t care. I’m not risking my mental health again. And if you think that’s ‘irrational’? You’ve never been the 1 out of 10.