Food Sensitivity & Constipation Tracker
Track Your Daily Intake
Log your food consumption and corresponding symptoms to identify patterns over time.
Your Pattern Analysis
Your symptoms and intake patterns will appear here after adding entries.
Personalized Guidance
Based on your entries, you should consider:
- Elimination diet phase Start in 2 weeks
- Key food to monitor Lactose
- Recommended next step Trial low-FODMAP foods
When you’re stuck with chronic idiopathic constipation (CIC), the frustration can feel endless. What makes it even trickier is that the cause isn’t always obvious - there’s often an unseen link to what you eat. In this guide we’ll uncover how food sensitivities can keep your bowels sluggish, show you how to spot the culprits, and give you practical steps to get things moving again.
Key Takeaways
- CIC often co‑exists with hidden food sensitivities that affect gut motility.
- Identifying trigger foods usually requires a structured elimination diet and symptom diary.
- Low‑FODMAP, fiber balancing, and targeted probiotics can improve both sensitivity and constipation.
- Monitoring and adjusting the plan over weeks is essential for lasting relief.
What is Chronic Idiopathic Constipation?
Chronic Idiopathic Constipation is a condition where bowel movements are infrequent, hard, or incomplete for at least three months without an identifiable medical cause. "Idiopathic" means doctors haven’t found a structural problem, infection, or medication that explains the slowdown.
Typical signs include fewer than three stools a week, straining, a feeling of incomplete emptying, and sometimes abdominal bloating. The real challenge is that the underlying mechanisms can vary widely from person to person.
Understanding Food Sensitivities
Food sensitivities are non‑allergic reactions that occur when the digestive system struggles to break down certain components, leading to inflammation or altered nerve signaling in the gut.
Unlike classic food allergies that involve the immune system’s IgE antibodies, sensitivities often involve the innate immune response, gut microbiota imbalance, or enzyme deficiencies. These subtle reactions can change how the colon contracts, making stools slower and drier.
How Sensitivities Slow the Colon
The colon moves waste along through coordinated muscle waves called peristalsis. When a sensitive food triggers inflammation or changes the osmotic balance, it can dampen these waves. Two key pathways are:
- Inflammatory signaling: Certain foods increase cytokine release, which can desensitize the enteric nervous system and reduce contraction strength.
- Water absorption: Fermentable carbs that aren’t fully digested pull water into the gut lumen. If the gut wall is inflamed, it may re‑absorb too much water, leaving stools hard.
Both pathways can turn a normally smooth transit into a sluggish crawl, especially when the baseline motility is already low, as it often is in CIC.
Common Sensitivity Triggers
Not every food will cause problems, but a handful show up again and again in research and real‑world case studies. Below is a quick snapshot of the most frequent offenders.
| Trigger | Typical Reaction | Impact on Constipation |
|---|---|---|
| Lactose | Gas, bloating, mild diarrhea | Fermentation draws water, may harden stool later |
| Gluten (non‑celiac) | Abdominal pain, fatigue | Inflammation slows colonic muscle activity |
| Fructose | Bloating, cramping | Excess osmotic load can increase water re‑absorption |
| FODMAP‑rich vegetables (e.g., cauliflower, onions) | Gas, fullness | Fermentation by gut bacteria slows transit |
| Artificial sweeteners (e.g., sorbitol) | Loose stools, bloating | Can disrupt microbiome balance, affecting motility |
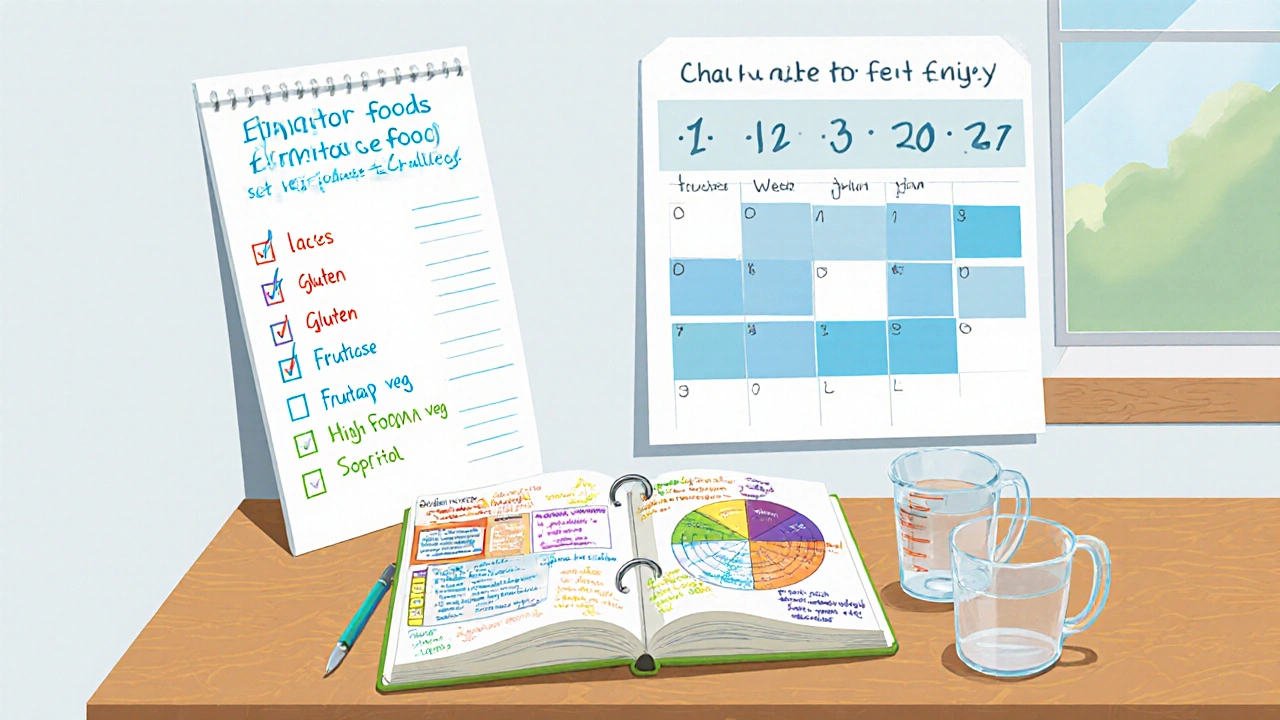
Getting Started: The Elimination‑Challenge Method
Finding your personal triggers doesn’t require a lab test; a well‑structured elimination diet does the trick for most people. Here’s a simple three‑phase plan you can follow at home.
- Eliminate (2‑4 weeks): Remove the top five foods from the table above. Keep a daily symptom log - note stool frequency, consistency (use the Bristol Stool Chart), bloating, and energy levels.
- Reintroduce (1‑2 weeks per food): Add one food back every five days while continuing the log. A clear worsening of symptoms points to a sensitivity.
- Challenge & Adjust (ongoing): Once you’ve identified triggers, decide whether you’ll avoid them completely, limit portions, or pair them with supportive foods (like probiotics).
This method works because it isolates variables and gives your gut time to reset. Consistency is key - sudden changes in stress, activity, or medication can mask results.
Dietary Strategies That Ease Constipation
After you know what to steer clear of, the next step is building a diet that encourages regularity.
- Low‑FODMAP diet - Limits fermentable carbs that feed gas‑producing bacteria. Many people with CIC see smoother transit within two weeks.
- Balanced fiber: Aim for 25‑30g per day, but split between soluble (oats, psyllium) and insoluble (whole grains, berries). Soluble fiber forms a gel that softens stool; insoluble adds bulk.
- Hydration: At least 1.5L of water daily, more if you’re active. Warm liquids in the morning can stimulate the gastrocolic reflex.
- Probiotics & prebiotics: Strains likeBifidobacteriuminfantisandLactobacillusplantarumhave research‑backed benefits for motility. Pair them with prebiotic fibers (e.g., inulin) to feed good bacteria.
- Magnesium‑rich foods: Nuts, seeds, leafy greens. Magnesium acts as a mild laxative by drawing water into the intestines.
Eating regular meals, rather than long gaps, also helps keep the colon rhythm steady. A 3‑hour eating window is a practical rule for many.
Beyond Food: Lifestyle Tweaks That Complement the Diet
Food is just one piece of the puzzle. Here are low‑effort habits that support a healthier gut.
- Move daily: Even a 15‑minute walk after meals can boost peristalsis.
- Stress management: Chronic stress raises cortisol, which can slow gut motility. Try breathing exercises, short yoga sessions, or mindfulness apps.
- Sleep hygiene: Aim for 7‑9 hours. Irregular sleep patterns interfere with the body’s circadian control of digestion.
When to Seek Professional Help
If you’ve tried elimination, diet changes, and lifestyle tweaks for eight weeks and still see fewer than three stools a week, it’s time to see a clinician. Possible next steps include:
- Motility testing (e.g., colonic transit study)
- Targeted bowel‑stimulating meds - osmotic laxatives, lubiprostone, or linaclotide
- Referral to a gastroenterology dietitian for a personalized plan
Never ignore red‑flag signs like sudden weight loss, blood in stool, or severe abdominal pain - those need immediate medical evaluation.
Putting It All Together: A Sample 4‑Week Plan
- Week1‑2 (Eliminate): Cut out lactose, gluten, fructose, high‑FODMAP veg, and sorbitol. Track stool frequency, consistency, and bloating.
- Week3 (Reintroduce): Add lactose‑containing foods (e.g., milk) for five days. If symptoms spike, label lactose as a trigger.
- Repeat for gluten, then fructose, then each FODMAP veg, then sweeteners.
- Week4 (Adjust): Keep identified triggers out or limited. Introduce low‑FODMAP foods, 25g balanced fiber, 1.7L water, and a probiotic capsule containing B.infantis.
By the end of the month most people notice more regular, softer stools and less abdominal discomfort. The key is to keep the diary - it tells you if a new food later on starts causing trouble again.
Bottom Line
Chronic idiopathic constipation isn’t a mystery you have to live with forever. Food sensitivities are a hidden driver that you can discover with a systematic approach, then tame with the right diet and simple lifestyle habits. Start with the elimination‑challenge method, add fiber and gut‑friendly nutrients, and monitor your progress. If stuck, a clinician can add advanced testing or medication. With patience and a bit of experimentation, you can break the cycle and get your gut back on track.
Frequently Asked Questions
Can I self‑diagnose food sensitivities without a doctor?
Yes, most people start with a structured elimination diet at home. Tracking symptoms carefully lets you spot patterns before seeking lab tests, which are usually reserved for ambiguous cases.
Why doesn’t a high‑fiber diet always help constipation?
If the fiber is mostly insoluble and you’re also sensitive to fermentable carbs, the extra bulk can actually slow things down. Balancing soluble and insoluble fiber, and reducing FODMAPs, is usually more effective.
Is it safe to take probiotics every day?
For most healthy adults, daily probiotic supplementation is safe. Choose strains with clinical backing for constipation, like Bifidobacterium infantis, and follow the label dosage.
How long does it take to see results after changing my diet?
Most people notice softer stools within 5‑7 days of adding more water and soluble fiber. Full symptom improvement, especially after eliminating triggers, can take 2‑4 weeks.
When should I see a doctor for chronic constipation?
If you’ve tried diet and lifestyle changes for eight weeks without consistent relief, or if you develop alarm signs like blood, severe pain, or unexplained weight loss, schedule a medical evaluation promptly.







Comments
tom tatomi
I doubt the low‑FODMAP claim actually helps everyone.
Tom Haymes
Starting an elimination diet can feel overwhelming, but think of it as a personal experiment in self‑care.
First, commit to a clear timeline; two weeks without the suspected triggers gives your gut a chance to reset.
During this period, keep a simple chart: date, foods eaten, stool consistency, and any bloating or discomfort.
When you reintroduce a food, do it on a single day and observe any changes for the next 48 hours before moving on.
If a particular item consistently worsens your symptoms, label it as a trigger and consider long‑term strategies-either avoidance or portion control.
Remember that stress and hydration also play a huge role; drinking a glass of warm water each morning can stimulate the gastrocolic reflex.
Fiber balance is key: soluble fiber like psyllium can soften stools, while insoluble fiber adds bulk; the right mix often prevents the pendulum swing between diarrhea and constipation.
Don’t forget probiotics; strains such as Bifidobacterium infantis have been shown to improve motility when paired with prebiotic‑rich foods.
Magnesium‑rich foods, for example, nuts and leafy greens, act as gentle laxatives by drawing water into the intestines.
While tracking, be honest with yourself-sometimes we overlook hidden sources of FODMAPs like certain sauces or processed snacks.
The goal isn’t perfection; it’s progress, and each data point brings you closer to a personalized plan.
If after several weeks you still see fewer than three stools a week, consider consulting a gastroenterology dietitian for a tailored approach.
Red‑flag symptoms-blood, severe pain, or rapid weight loss-should prompt immediate medical attention.
Above all, stay patient; your gut ecosystem takes time to adapt, and consistency will eventually reward you with more regular, comfortable bowel movements.
Scott Kohler
It is rather amusing how the mainstream nutrition community loves to slap a single label-"low‑FODMAP"-on a complex physiological issue.
One must wonder whether the push for such simplified solutions is motivated by genuine science or by commercial interests.
Nevertheless, the data on inflammatory signaling and water absorption pathways remain compelling, albeit under‑reported.
Proceed with caution, and verify any dietary shift with a qualified professional.
Brittany McGuigan
Honestly this whole "food sensitivity" talk is just a trendy excuse for people who cant handle spicys food.
We need more real science not hype, and stop follwing every new diet fad.
Our bodies are stronger then we think.
Priya Vadivel
Thank you for the thorough breakdown, especially the emphasis on keeping a symptom log; I find that meticulous tracking can reveal patterns that are otherwise invisible, and it encourages a sense of empowerment over one’s own health, which is so important,
Also, the reminder about stress and sleep resonates with me, as I’ve noticed my bowel habits worsen during hectic weeks, and a consistent bedtime can make a noticeable difference.
Dharmraj Kevat
Eliminate the junk, watch the gut.
Simple as that.
Jennifer Boyd
Hey folks, this guide is like a lighthouse in a foggy sea of constipation!
Stick to the plan, stay hydrated, and celebrate every tiny win-like that first soft stool after a week of effort.
Remember, patience is your best ally; the gut loves consistency.
We’ve all been there, and together we’ll get moving again.
Lauren DiSabato
While the article offers a decent overview, it overlooks the nuanced role of gut‑brain axis signaling beyond mere fiber intake.
In practice, merely swapping out FODMAPs without addressing underlying dysbiosis may yield temporary relief at best.
Hutchins Harbin
Great points on magnesium and probiotics-those are often the missing pieces in many constipation plans.
One thing to add: timing matters. Taking magnesium at night can help synchronize the colon’s natural nocturnal activity.
Also, choose a probiotic with at least 10 billion CFU to ensure enough viable organisms survive stomach acid.
Don’t forget to pair prebiotic fibers; they feed the good bacteria and enhance their effect on motility.
Finally, keep an eye on any new symptoms after reintroducing foods; subtle changes can signal emerging sensitivities.
Benjamin Herod
Honestly, the article reads like a checklist that anyone can copy‑paste without understanding the why.
It’s a good start, but real change demands deeper introspection.
Let’s not forget the power of movement after meals-just a short walk can make a world of difference.
luemba leonardo brás kali
The emphasis on a balanced fiber ratio is spot‑on; many people over‑consume insoluble fiber, worsening constipation.
Soluble fibers like psyllium form a gel that retains water, softening stools, while insoluble fibers add bulk without absorbing excess moisture.
Integrating both types, alongside adequate hydration, creates an optimal environment for peristalsis.
Precision in diet composition is essential for sustainable relief.
Corey McGhie
Nice job breaking down the elimination‑challenge method-it's practically a DIY clinical trial.
Just a heads‑up: some folks experience mild withdrawal symptoms when cutting out sugar substitutes like sorbitol, so expect a short adjustment period.
Also, keep the probiotic capsule handy; consistency is key, otherwise you’ll lose the momentum you built.
Remember, the gut loves regular meals-try a 3‑hour eating window to keep the colon rhythm steady.
Overall, solid advice with enough flexibility to fit most lifestyles.
Terry Duke
Interesting take on stress management; I’ve found that even a five‑minute breathing exercise can kick‑start peristalsis.
Coupling that with a morning warm beverage seems to amplify the effect, especially for those with erratic schedules.
Staying active after meals, even a brief stroll, reinforces the gastrocolic reflex.
All these small habits add up to noticeable improvement over weeks.
Chester Bennett
The recommendation to seek professional help after eight weeks is prudent; persistent constipation can signal deeper motility disorders.
However, before that point, a simple home‑based bowel‑stimulating routine-like sipping warm water with lemon each morning-can be quite effective.
It’s also wise to monitor any red‑flag symptoms carefully, as early detection matters.
Overall, the guide balances self‑management with appropriate medical escalation.
Samantha Leong
I appreciate the calm, thorough tone of the article; it makes a daunting topic feel manageable.
The step‑by‑step elimination plan is especially helpful for readers who might feel lost without clear guidance.
Adding reminders about hydration and sleep reinforces that constipation isn’t just a gut issue, but a whole‑body concern.
Thanks for the comprehensive resource.
carlee Lee
This is a solid, practical guide.
Follow it and you’ll likely see improvement.
chuck thomas
The interplay between inflammation and peristalsis is a fascinating aspect that many overlook.
Understanding how specific food components alter osmotic balance helps explain why some patients respond dramatically to low‑FODMAP diets.
Moreover, integrating probiotics with prebiotic fibers creates a synergistic environment for gut motility.
It’s also worth noting that individual variability means the elimination phase may need adjustment based on symptom severity.
Overall, the article presents a balanced, evidence‑based roadmap for tackling chronic idiopathic constipation.