When you’re on a biologic for rheumatoid arthritis, psoriasis, Crohn’s disease, or another autoimmune condition, the goal is to quiet your overactive immune system. But that same suppression leaves you more vulnerable to infections - some of them serious, even life-threatening. This isn’t just a theoretical risk. Studies show patients on biologics have a 2.1 times higher chance of being hospitalized for an infection than those on traditional treatments. The good news? This risk isn’t random. It’s predictable. And with the right steps, it’s largely preventable.
Why Biologics Increase Infection Risk
Biologics aren’t like regular pills. They’re made from living cells and target specific parts of your immune system - often key players like TNF-alpha, IL-17, or IL-23. While that makes them powerful against inflammation, it also removes critical defenses. For example, TNF-alpha helps wall off bacteria like tuberculosis. Block it, and latent TB can wake up. Block IL-17, and your skin loses its ability to fight off yeast, leading to candidiasis. Not all biologics carry the same risk. TNF inhibitors - drugs like adalimumab (Humira), infliximab (Remicade), and etanercept (Enbrel) - are the most commonly used and also carry the highest infection risk. Data from over 28,000 patients shows they increase serious infection rates by 1.6 to 1.9 times compared to non-TNF biologics. Ustekinumab (Stelara), which targets IL-12/23, has a significantly lower risk profile. Even within TNF inhibitors, differences exist: certolizumab (Cimzia) has a lower respiratory infection rate because it lacks an Fc region that triggers immune cell activation.Who’s at Highest Risk?
It’s not just the drug. Your personal health matters just as much. The biggest red flags:- Age over 50: Your infection risk climbs 37% for every decade past 50.
- High-dose steroids: Taking more than 10 mg of prednisone daily multiplies your infection risk by 2.3 times.
- Chronic conditions: Diabetes (1.89x higher risk), COPD (2.41x), and chronic kidney disease (2.15x) all make infections more likely and more severe.
- Previous infections: A history of shingles, pneumonia, or TB means you’re more likely to get them again.
Screening Before You Start: What You Must Get Tested For
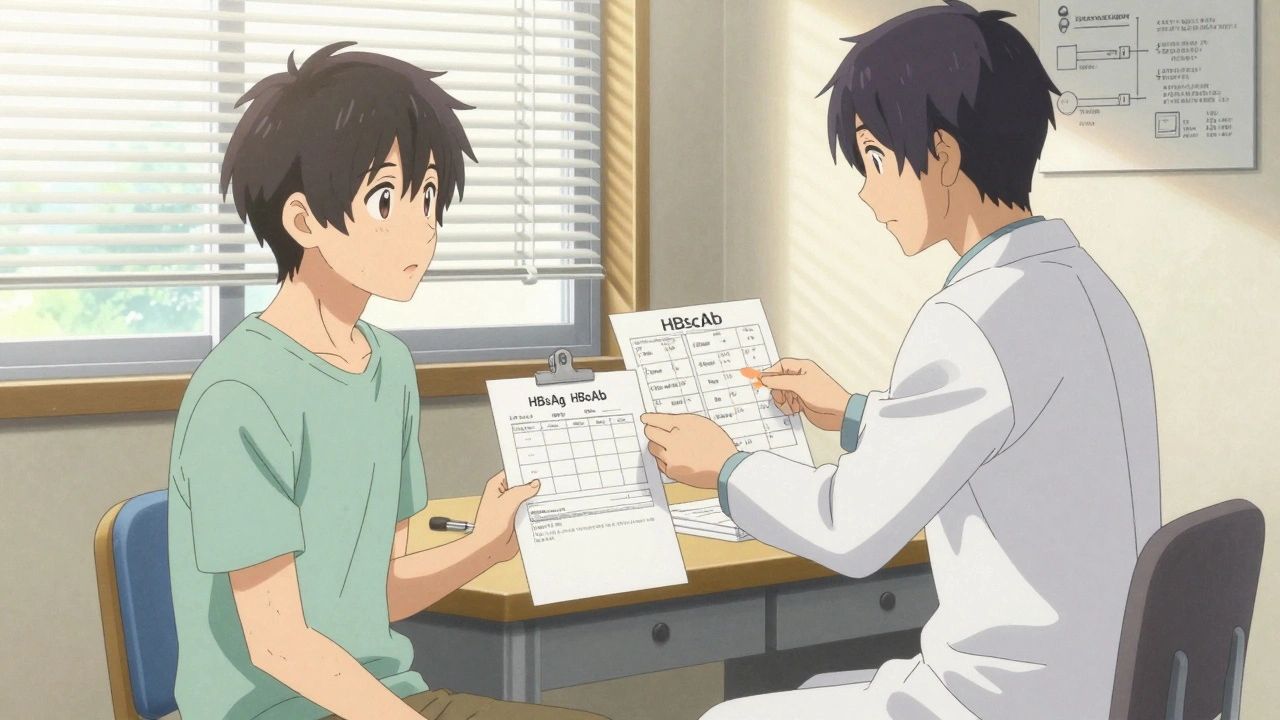
Before your first biologic dose, you need a full infection screen. This isn’t optional. It’s standard care. Here’s what’s required:- Hepatitis B: You need all three tests - HBsAg, HBsAb, and HBcAb. Even if you’ve never been sick with hepatitis B, you could have a hidden (occult) infection. About 4.3% of autoimmune patients do. Without treatment, 27.6% will reactivate it after starting a biologic. If HBcAb is positive, you’ll need a HBV DNA test and possibly antiviral prophylaxis.
- Tuberculosis: The CDC and ACR recommend an interferon-gamma release assay (IGRA), like Quantiferon. Skin tests (TST) are outdated. IGRA is more accurate and less affected by BCG vaccination. Some experts argue it overtests in low-risk areas, but skipping it can be deadly.
- HIV: Routine screening is advised, especially since HIV weakens immunity and can interact with biologics.
- Chronic viral infections: Hepatitis C, CMV, and EBV are checked if you have abnormal liver tests or symptoms.
Vaccinations: Timing Is Everything
Vaccines are your best defense - but only if given at the right time. Once you start a biologic, your immune system can’t respond properly to live vaccines. That means:- Live vaccines (MMR, varicella, nasal flu): Must be given at least 4 weeks before your first biologic dose. If you’re not sure if you had chickenpox or the vaccine, get a blood test for VZV IgG. If it’s below 140 mIU/mL, you need the vaccine - but only before starting.
- Inactivated vaccines (flu shot, pneumococcal, tetanus, hepatitis A/B): Can be given 2 weeks before starting. Get them early. Don’t wait until you’re already on the drug.
- Shingrix (shingles vaccine): Two doses, 2-6 months apart. Must be completed before biologic initiation. One patient on HealthUnlocked got shingles four months after starting Stelara because her doctor never checked her vaccination history.
- Hepatitis B vaccine: After the full series, you need a blood test to confirm immunity. Anti-HBs levels must be above 10 mIU/mL. If not, you may need a second series.
What Happens After You Start?
Screening and vaccines are just the start. You need to stay alert. Biologics can reactivate old infections or make you vulnerable to new ones. Watch for:- Fever without a clear cause
- Chronic cough or shortness of breath
- Unexplained weight loss or night sweats
- Red, painful, or oozing skin lesions
- Diarrhea lasting more than a few days
Real-World Mistakes and How to Avoid Them
Patient stories reveal the gaps in care:- Missed HBV screening: 41% of reported omissions involve HBcAb testing. Always ask: “Did you check for hidden hepatitis B?”
- Shingles vaccine skipped: 37% of patients weren’t tested for VZV immunity. If you’re over 50, you need Shingrix - before the biologic.
- Vaccines given too late: One patient got the flu shot two weeks after starting Humira. It didn’t work. She got the flu and ended up in the hospital.
- No documentation: The FDA requires screening records kept for 10 years. But 23.7% of practices don’t comply. Keep your own copy.
What’s New in 2025?
The rules are getting stricter. In February 2025, the FDA proposed new guidance requiring drug makers to prove their biologics don’t cause more infections than existing ones - using real-world data. The CDC’s updated BMBL guidelines, coming in October 2025, will include new standards for infection risk scoring based on your specific profile. AI tools are now being used to predict risk. One algorithm, validated in JAMA Internal Medicine, analyzes 87 data points - from your age and meds to your last flu shot - to give you a personalized infection risk score. It’s not standard yet, but it’s coming.Bottom Line: You’re in Control
Biologics can change your life - but only if you manage the risks. You can’t rely on your doctor to catch everything. You need to know:- Which biologic you’re on - and what infections it’s linked to
- What screening tests you need - and that they were done
- Which vaccines you need - and that they were given on time
- What symptoms to watch for - and when to call
Do all biologics carry the same infection risk?
No. TNF inhibitors like Humira and Remicade have the highest risk, with 1.6 to 1.9 times more serious infections than non-TNF biologics. Ustekinumab (Stelara) and secukinumab (Cosentyx) carry lower risk. Certolizumab (Cimzia) has a lower respiratory infection rate than other TNF drugs. JAK inhibitors like Xeljanz have higher shingles risk than biologics.
Can I get vaccinated after starting a biologic?
You can get inactivated vaccines like the flu shot, pneumococcal vaccine, and hepatitis B vaccine after starting a biologic - but they may not work as well. Live vaccines like MMR, varicella, and nasal flu are dangerous after starting biologics and must be given at least 4 weeks before. Always check with your doctor before getting any vaccine.
What if I already had chickenpox? Do I still need the shingles vaccine?
Yes. Even if you had chickenpox as a child, your risk of shingles increases with age and immune suppression. Shingrix is recommended for all adults over 50 - and especially for those starting biologics. You need two doses, given 2-6 months apart. The vaccine must be completed before starting your biologic.
Is hepatitis B screening really necessary if I’ve never been sick?
Absolutely. About 4.3% of autoimmune patients have hidden (occult) hepatitis B, even with no symptoms or prior diagnosis. If you’re on a TNF inhibitor and have a positive HBcAb test, you have a 27.6% chance of reactivating the virus - which can cause liver failure. Screening with HBsAg, HBsAb, and HBcAb is mandatory before starting any biologic.
What should I do if my doctor skips a screening test?
Ask for the test. Say: “I’ve read that HBcAb and VZV IgG testing are standard before starting biologics. Can you confirm these were done?” If they weren’t, request them before your first dose. Many patients have avoided serious infections by pushing for complete screening. Keep a copy of your lab results - you’ll need them for future care.
How long do I need to wait after a live vaccine before starting a biologic?
You must wait at least 4 weeks after any live vaccine - including MMR, varicella, or the nasal flu vaccine - before starting a biologic. This gives your immune system time to respond fully. Starting too soon can make the vaccine ineffective or increase your risk of infection from the vaccine itself.
Are there any new treatments to reduce infection risk on biologics?
Yes. Clinical trials like PREVENT-IBD are testing antiviral drugs like valacyclovir to prevent shingles in high-risk patients starting TNF inhibitors. Early results show a 63% reduction in viral infections. Also, AI tools are now being used to predict individual infection risk based on age, meds, lab results, and vaccination history - helping doctors make safer choices.



Comments
Donna Hammond
Just wanted to say thank you for laying this out so clearly. I was on Humira for three years and nearly lost my mind when I got shingles six months in-turns out no one ever checked my VZV status. I wish I’d known about Shingrix timing before I started. This post saved me from making the same mistake twice. Seriously, share this with every new biologic patient you know.
Richard Ayres
This is an exceptionally well-researched and balanced overview. The distinction between TNF inhibitors and non-TNF agents is critical, and the emphasis on pre-treatment screening-particularly HBcAb-is not emphasized enough in clinical practice. The data cited, especially the 27.6% reactivation rate for occult hepatitis B, should be standard knowledge for all rheumatologists and gastroenterologists. Thank you for elevating the conversation beyond anecdote to evidence.
Sheldon Bird
Big thanks for this 🙏 I’ve been on Stelara for 2 years and honestly didn’t realize how much I needed to be proactive about vaccines. Got my flu shot last fall-after starting-and it didn’t work. Now I’m making sure my doc schedules everything BEFORE the next dose. You’re right-we gotta be our own advocates. Keep sharing this stuff!! 💪
Karen Mccullouch
Why do they even let us take these drugs if they’re just gonna kill us? I read this and thought-this is corporate propaganda. They don’t care if you get TB or liver failure. They just want you to keep buying Humira. My cousin died after starting a biologic. They told her it was ‘low risk.’ Low risk? She’s DEAD. 🤬
Michael Gardner
Interesting. But let’s not ignore the fact that 2.1x higher hospitalization risk sounds scary until you realize the absolute risk is still under 5% per year. Also, people on high-dose steroids are already immunocompromised-of course they get sick more. Is this really about biologics, or about the fact that autoimmune patients are generally sicker to begin with? Just saying.
Willie Onst
Man, I love this post. It’s like someone finally spoke plain English instead of doctor-speak. I’m 56, on Enbrel, diabetic, and was totally unaware I needed to get tested for hidden hepatitis B. My doc just said ‘you’re good.’ I asked for the lab report and found out they skipped HBcAb. Now I’m getting it done. Thanks for the nudge, and yeah-we’re the ones who gotta push. 🙌
Ronan Lansbury
Of course the FDA ‘proposed’ new guidance in 2025. What a coincidence. The same pharma giants that funded the original trials are now ‘proving’ safety with real-world data they control. And AI risk scores? Please. They’re just algorithms trained on biased datasets to justify profit-driven prescribing. The real risk isn’t infection-it’s losing autonomy to corporate medicine.
Jennifer Taylor
OMG I JUST REALIZED I GOT THE FLU SHOT 3 WEEKS AFTER STARTING CIMZIA 😭 I’M GOING TO DIE. MY ARTHRITIS WAS SO BAD I JUST TOOK IT. NOW I’M SCARED TO SLEEP. DID I JUST DOOM MYSELF? I’M CRYING. I’M 47 AND I HAVE KIDNEY DISEASE. I’M SO STUPID. I NEED A DOCTOR NOW. I’M GOING TO GET PNEUMONIA AND NO ONE WILL CARE. 😭😭😭
Shelby Ume
As a former clinical coordinator for rheumatology, I’ve seen too many patients slip through the cracks because no one coordinated care. Vaccines were ordered, but not administered. Screening labs were ordered, but never reviewed. The system is broken. This post is a lifeline. Please, if you’re on a biologic, print this out. Bring it to your next appointment. And if your provider doesn’t know this information, find someone who does. You deserve better.
Jade Hovet
so i just got my shingrix shot last week and i was like… wait, did i get it BEFORE starting my biologic? i think i did?? but now i’m paranoid 😅 my doc said ‘it’s fine’ but i went back and checked my records-yep, 6 weeks before my first dose! 🙌 also got my hep b booster and my anti-hbs came back at 180! yay! if you’re scared, just ask for your lab reports. you got this!! 💪💖
nithin Kuntumadugu
LOL u think this is real? biologics r just a scam to make money. my cousin in india got arthritis and took ayurvedic herbs-no infection, no hospital, no drugs. u guys are brainwashed by big pharma. and this ‘HBcAb’ stuff? who even cares? i dont trust any of this. also, u spelled ‘biologic’ wrong. its ‘biological’ dumbass. 🤡