Vitamin K Consistency Calculator
Track Your Vitamin K Intake
Calculate your daily vitamin K intake from common foods to stay within the recommended range of 90-120 µg for stable warfarin therapy.
Your Daily Vitamin K Intake
Recommended Daily Range
Most people on warfarin should aim for 90-120 µg of vitamin K per day to maintain stable INR levels without major fluctuations.
Aim for the middle of this range (105 µg) for best stability.
When you're on warfarin, your body is caught in a quiet balancing act. One day you eat a big salad, your INR drops. The next day you skip the greens, your INR spikes. It’s not magic - it’s vitamin K. This simple nutrient in leafy greens directly fights warfarin’s effect, and how much you eat every day can mean the difference between a safe clot-free day and a trip to the ER.
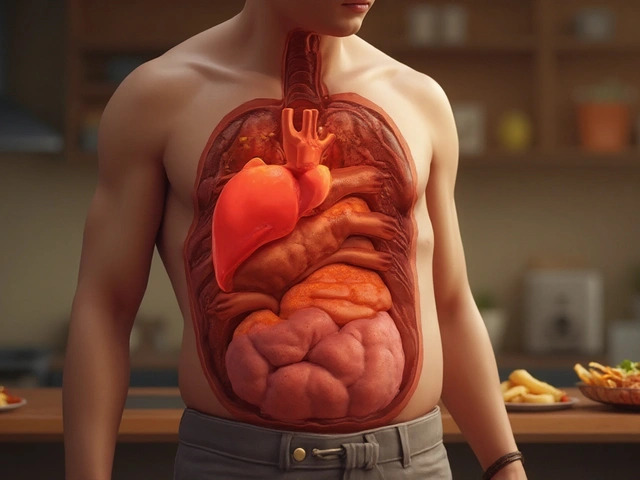
Why Vitamin K Matters More Than You Think
Warfarin doesn’t just thin your blood - it blocks vitamin K from doing its job. Vitamin K helps your liver make clotting factors. Without it, your blood takes longer to clot. That’s good if you’re at risk for a stroke or clot. But if you suddenly eat a lot of vitamin K, your body can make those clotting factors again. Your INR plummets. That’s dangerous. If you eat almost no vitamin K for days, your INR rises too high. That’s also dangerous.
It’s not about avoiding vitamin K. It’s about consistency. The American Heart Association, the American College of Cardiology, and the American Society of Hematology all agree: don’t cut out greens. Don’t go on a low-K diet. Just eat about the same amount every day.
What Foods Have the Most Vitamin K?
Not all vegetables are equal. Some pack a punch. Others barely register. Here’s what you need to know:
- Cooked spinach: 889 µg per cup - that’s nearly 8 times the daily recommended intake for a healthy adult.
- Cooked kale: 547 µg per cup - a single serving can throw off your INR if you’re not used to it.
- Cooked collard greens: 772 µg per cup - one of the highest sources.
- Cooked broccoli: 220 µg per cup - still high, but easier to manage.
- Asparagus: 70 µg per half-cup - moderate, safe with occasional variation.
- Green beans: 14 µg per half-cup - very low risk.
Raw spinach? About 145 µg per cup. Cooked? Almost 900 µg. Cooking concentrates vitamin K by removing water. That’s why a salad one day and sautéed greens the next can cause wild INR swings.
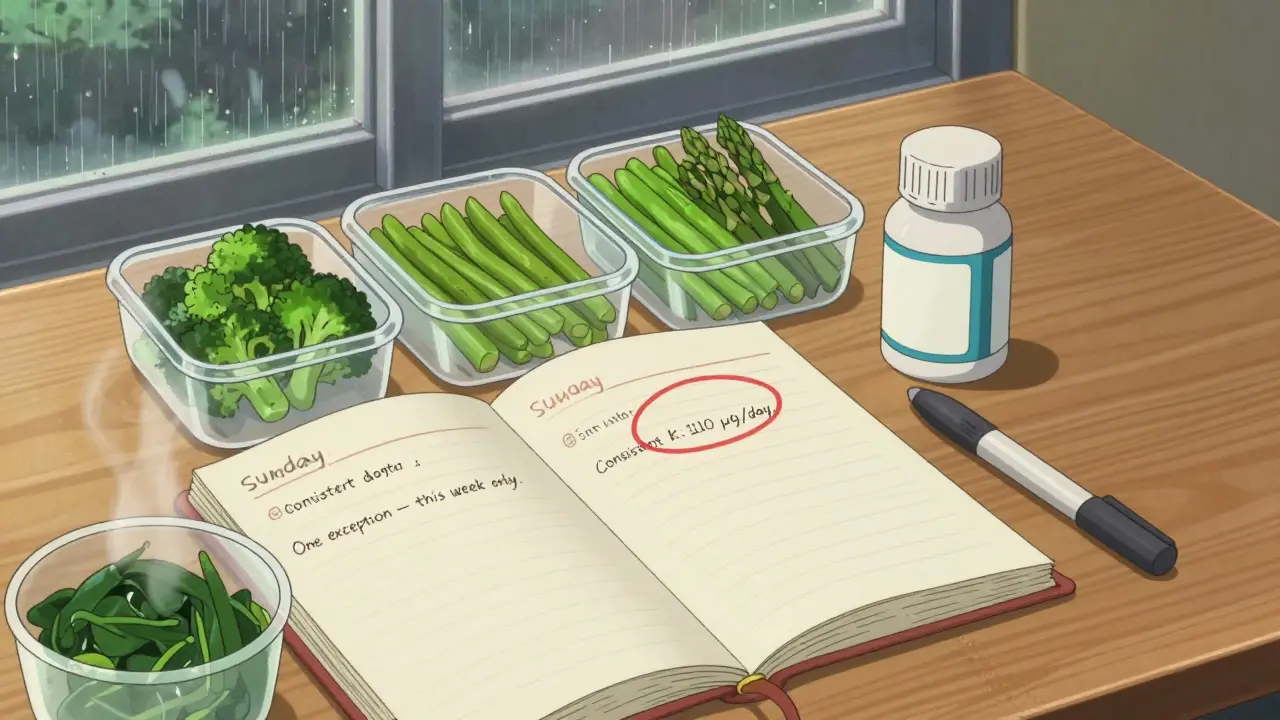
How Much Is Too Much? The Sweet Spot
You don’t need to count every microgram. But you do need a target. Most experts recommend staying between 90 and 120 µg of vitamin K per day. That’s the range most people on warfarin can handle without major INR swings.
Here’s what that looks like in real meals:
- One cup of raw spinach (145 µg) - a little high, but okay if you eat it every day.
- Half a cup of cooked broccoli (110 µg) - perfect daily amount.
- One cup of green beans (28 µg) + half a cup of asparagus (35 µg) = 63 µg - safe and stable.
Don’t panic if you eat a big serving of kale once. The problem isn’t the occasional cheat. It’s the pattern. If you normally eat one serving of greens, then suddenly eat three, your INR can crash in 2-3 days. If you normally eat three, then skip for a week, your INR can spike. Consistency beats perfection.
What About Other Sources of Vitamin K?
It’s not just vegetables. Some supplements and processed foods sneak in vitamin K:
- Meal replacement shakes like Ensure® (50 µg per serving) and Boost® (55 µg) - check labels.
- Multivitamins - many contain 50-100 µg of vitamin K. If you take one, make sure it’s the same every day.
- Fermented foods like natto, sauerkraut, and cheese contain vitamin K2. It’s less studied, but if you eat it regularly, keep eating it. If you don’t, don’t start.
Antibiotics can also change your vitamin K levels. Your gut bacteria make some vitamin K2. When antibiotics kill those bacteria, your body makes less. That can raise your INR. If you’re on antibiotics, tell your anticoagulation clinic. They may adjust your warfarin dose.
What Happens When You Don’t Stay Consistent?
Real stories tell the truth.
One patient on the American Heart Association’s forum said: “I ate one cup of baby spinach every morning. My INR went from unstable (TTR 52%) to rock solid (81%) in six months.”
Another Reddit user wrote: “I had a kale salad for lunch - three servings. I normally eat zero. My INR dropped from 2.5 to 1.8 overnight. They had to increase my warfarin dose. I was scared.”
These aren’t rare. A 2022 study found 63% of patients got conflicting advice from different doctors. Some were told to avoid all greens. Others were told to eat more. That confusion leads to bad outcomes.
How to Build a Consistent Routine
Stability doesn’t happen by accident. Here’s how to make it stick:
- Choose one high-K food and eat the same portion every day. Spinach, broccoli, or kale - pick one. Not all of them.
- Use a food diary or app. MyFitnessPal has a vitamin K tracker. INR Tracker Pro is used by clinics. Log what you eat.
- Plan meals weekly. Cook your greens on Sunday. Eat the same amount each day. No surprises.
- Don’t start new supplements without checking with your doctor. Even “natural” ones can have vitamin K.
- Know your INR trend. If your INR is dropping, check your food. If it’s rising, check for illness, antibiotics, or skipped meals.
It takes 8 to 12 weeks to build this habit. But once you do, your INR stays in range 75-80% of the time. That’s way better than the 55-65% most people get with inconsistent eating.
Why Warfarin Still Matters
There are newer blood thinners - apixaban, rivaroxaban, dabigatran. They don’t care what you eat. But they cost $3,500 a year. Warfarin costs $4-$10. For millions, that’s the difference between taking it and not taking it.
And here’s the truth: if you can manage your diet, warfarin works better than most people think. It’s reversible. If you bleed, vitamin K or fresh frozen plasma can save you. Newer drugs don’t have that safety net.
That’s why 35% of new atrial fibrillation patients still get warfarin in 2026. Not because it’s outdated. Because when used right - with consistent vitamin K - it’s one of the most reliable tools we have.
What to Avoid
- Extreme diets - keto, vegan, raw food - if they change your vitamin K intake drastically.
- Unsupervised supplements - even “natural” vitamin K pills can spike your levels.
- Guessing - if you don’t know how much vitamin K is in a food, assume it’s high and avoid it until you check.
- Skipping meals - if you’re sick and eat less, your INR can rise. Tell your clinic.
Can I eat spinach if I’m on warfarin?
Yes - but only if you eat the same amount every day. One cup of raw spinach (145 µg) is fine if you have it daily. But if you eat it once a week and then suddenly eat it every day, your INR will drop. Consistency matters more than the food itself.
Should I avoid all green vegetables?
No. Avoiding all greens is outdated advice and can be harmful. Studies show patients who restrict vitamin K have more INR swings because they eat it inconsistently. The goal is not to eliminate vitamin K - it’s to keep it steady. Eat a small, consistent amount every day.
Does cooking affect vitamin K levels?
Yes - dramatically. Raw spinach has about 145 µg per cup. Cooked spinach has 889 µg. That’s because cooking removes water, concentrating the vitamin K. If you normally eat raw, don’t switch to cooked without telling your doctor. Same goes for kale, broccoli, and collards.
What if I’m on antibiotics?
Antibiotics can reduce your body’s natural production of vitamin K2 from gut bacteria. This can cause your INR to rise. If you’re on antibiotics for more than a few days, notify your anticoagulation clinic. They may need to adjust your warfarin dose temporarily.
Is vitamin K supplementation helpful?
Yes - for some. A 2020 study found that patients with unstable INRs who took 100-150 µg of vitamin K daily had better stability than those who avoided it. This isn’t for everyone, but if your INR is all over the place despite diet consistency, talk to your doctor about a low-dose supplement. Don’t self-prescribe.
Final Thought
You’re not trying to eat perfectly. You’re trying to eat predictably. Warfarin works best when your body knows what to expect. One cup of spinach every morning. One serving of broccoli every night. No surprises. No extremes. That’s the secret. Not fear. Not restriction. Just routine.