Lopinavir/Ritonavir Drug Interaction Checker
Check Medication Interactions
Enter a drug name to see if it interacts dangerously with lopinavir/ritonavir. Based on article information from the Liverpool HIV Interactions Database.
When you take lopinavir/ritonavir (Kaletra), you’re not just getting two drugs-you’re stepping into a complex chemical tug-of-war inside your liver. Ritonavir, given in a tiny dose, doesn’t treat HIV. Instead, it acts like a molecular shield, blocking the enzyme CYP3A4 from breaking down lopinavir. This trick, called pharmacokinetic boosting, lets lopinavir stay in your system longer at effective levels. But here’s the catch: CYP3A4 doesn’t just process lopinavir. It handles more than half of all prescription drugs. That means ritonavir’s shield doesn’t just protect lopinavir-it throws the whole metabolic system out of balance.
How Ritonavir Turns Off the Liver’s Cleanup Crew
CYP3A4 is the most active enzyme in your liver for breaking down medications. Think of it as the main garbage disposal for drugs. Lopinavir, on its own, gets shredded by CYP3A4 in minutes. Without help, you’d need to take it three times a day just to keep enough in your blood to fight HIV. Ritonavir changes that. It doesn’t just block CYP3A4-it permanently disables it. The enzyme binds to ritonavir, gets damaged, and stops working. This is called mechanism-based inactivation. Unlike simple blockers that come and go, ritonavir’s damage lasts until your liver makes new enzymes, which takes days.
Studies show that with ritonavir present, lopinavir’s metabolic clearance drops to less than 15% of what it would be alone. That’s why a 100mg dose of ritonavir can boost lopinavir levels by more than 500%. But this same power makes ritonavir one of the most dangerous drugs to mix with others. It doesn’t just inhibit CYP3A4-it also induces other enzymes like CYP1A2 and CYP2C9. That means it can both raise and lower drug levels depending on the pathway. One drug might build up to toxic levels, while another gets flushed out too fast.
Drugs That Can Kill You When Mixed With Lopinavir/Ritonavir
The Liverpool HIV Interactions Database tracks over 1,200 potential drug interactions with lopinavir/ritonavir. That’s more than double what you’ll find with newer regimens like darunavir/cobicistat. Some of these aren’t just side effects-they’re life-threatening.
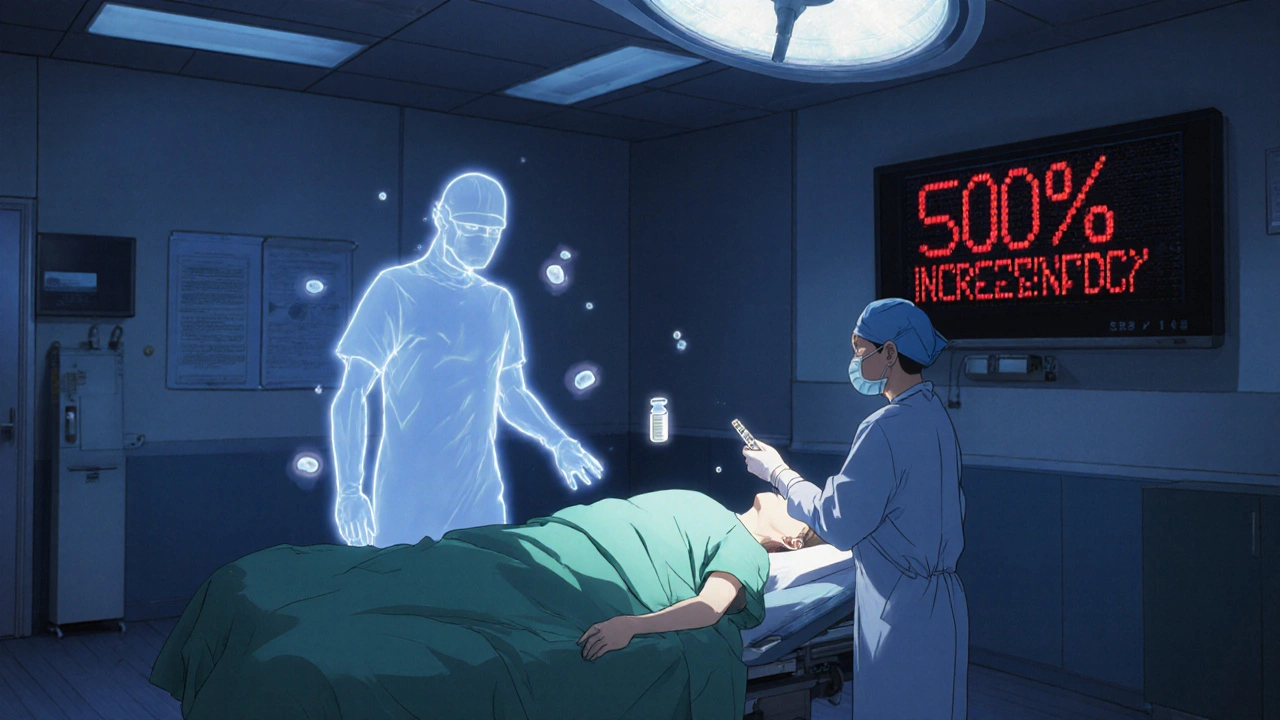
- Midazolam: Used for sedation before surgery. Ritonavir can increase its blood levels by 500%. A normal dose becomes a near-lethal overdose. Anesthesiologists must reduce it by 60-80%.
- Fentanyl: This opioid painkiller sees a 300% spike in concentration. Even small doses can cause fatal respiratory depression.
- Rivaroxaban: A blood thinner. Ritonavir increases its levels so much that the risk of internal bleeding skyrockets. It’s outright contraindicated.
- Tacrolimus: Used after organ transplants. Without a 75% dose reduction, patients risk kidney failure.
- Warfarin: Ritonavir induces CYP2C9, which breaks down warfarin faster. INR levels drop, raising the risk of clots-then suddenly spike when ritonavir is stopped.
- Statins: Simvastatin and lovastatin can cause rhabdomyolysis (muscle death) when boosted. Atorvastatin is safer but still needs monitoring.
- Hormonal contraceptives: Ritonavir cuts estrogen levels by 50%. Birth control pills become unreliable. Backup methods aren’t optional-they’re essential.
Even common OTC drugs like St. John’s wort can cause problems. It induces CYP3A4, which fights against ritonavir’s effect. The result? Lopinavir levels crash, and HIV rebounds.
Why Newer Drugs Are Replacing Lopinavir/Ritonavir
By 2023, lopinavir/ritonavir was used in less than 5% of new HIV starts in the U.S. Why? Because newer drugs don’t come with this minefield. Dolutegravir, bictegravir, and darunavir/cobicistat work just as well-but without ritonavir’s chaotic enzyme effects.
Cobicistat, the boosting agent in newer combos, only blocks CYP3A4. It doesn’t induce other enzymes. That makes its interaction profile predictable. A patient on darunavir/cobicistat might have 892 potential drug interactions. Lopinavir/ritonavir? 1,247. That’s not just more-it’s exponentially harder to manage.
Real-world data backs this up. A 2022 meta-analysis found patients on lopinavir/ritonavir were 37% more likely to stop treatment because of side effects like nausea, diarrhea, and liver damage. In contrast, integrase inhibitors like dolutegravir have fewer than 10% discontinuation rates due to toxicity.
Even in resource-limited settings, where lopinavir/ritonavir was once the go-to because of its low cost ($68 per person per year), the tide is turning. Dolutegravir is now available for under $100/year, and its simpler profile means fewer clinic visits, fewer lab tests, and fewer hospitalizations.
What Happens When You Skip the Interaction Check
Many clinicians still prescribe lopinavir/ritonavir without running a full drug interaction screen. That’s a mistake with serious consequences.
A 2008 study showed that when patients on lopinavir/ritonavir took rifampicin (a TB drug), their lopinavir levels dropped by 76%. That’s not just reduced effectiveness-it’s a direct path to drug-resistant HIV. At the same time, liver damage jumped from 11% to 33%.
One case involved a 42-year-old man on lopinavir/ritonavir who was prescribed a standard dose of fentanyl for post-surgery pain. He stopped breathing overnight. He survived, but only because staff caught it in time. His chart showed no mention of his HIV meds in the anesthesia notes.
Another patient on warfarin had stable INRs for months. After starting lopinavir/ritonavir, her INR dropped from 2.8 to 1.4 in two weeks. She developed a pulmonary embolism. Her doctor didn’t know ritonavir induces CYP2C9-the enzyme that breaks down warfarin.
These aren’t rare cases. They’re preventable.
How to Safely Use Lopinavir/Ritonavir Today
If you’re still on lopinavir/ritonavir-whether because of cost, access, or long-term use-here’s what you need to do:
- Run every medication through the Liverpool HIV Interactions Database. It’s free, updated monthly, and used by over 2.8 million clinicians annually. Don’t guess. Don’t rely on memory.
- Check for dual effects. If a drug is metabolized by CYP3A4, it might rise. If it’s metabolized by CYP2C9 or CYP1A2, it might fall. Ritonavir does both.
- Never start a new drug without reviewing interactions. Even antibiotics, antifungals, or acid reducers can interfere.
- Use alternatives where possible. For pain, avoid fentanyl and midazolam. Use acetaminophen or non-opioid options. For sleep, avoid benzodiazepines. Try melatonin or cognitive behavioral therapy.
- Monitor liver enzymes and INR regularly. If you’re on warfarin, check INR weekly for the first month after starting lopinavir/ritonavir.
- Use backup contraception. Hormonal birth control won’t work reliably. Use condoms, IUDs, or implants.
Dosing adjustments are critical. For patients with moderate liver damage (Child-Pugh Class B), the dose drops to 400/100mg once daily. For severe damage (Class C), don’t use it at all.
The Bigger Picture: Why This Matters Beyond HIV
Lopinavir/ritonavir isn’t just an HIV drug. It’s the blueprint for how we boost antivirals. That’s why ritonavir is in Paxlovid, the COVID-19 treatment. But even there, problems popped up. Some patients had "Paxlovid rebound"-their symptoms returned after treatment ended. Why? Because ritonavir’s CYP3A4 inhibition lasted longer than nirmatrelvir’s antiviral effect. Once ritonavir cleared, the body started breaking down nirmatrelvir too fast.
This same issue could affect future drugs. Every time we use ritonavir to boost a drug, we’re trading short-term effectiveness for long-term complexity. That’s why researchers are now studying CYP3A5 gene variants. Some people naturally have more of this enzyme. Early data shows they clear lopinavir 28% faster, meaning standard doses may not work for them.
The future of boosting is moving toward selective inhibitors like cobicistat-or even better, drugs that don’t need boosting at all. But until then, lopinavir/ritonavir remains a powerful tool with dangerous side effects. Knowing how CYP3A4 interacts with every other drug in your regimen isn’t optional. It’s the difference between staying healthy and ending up in the ER.
Can I take ibuprofen with lopinavir/ritonavir?
Yes, ibuprofen is generally safe to take with lopinavir/ritonavir. It’s not metabolized by CYP3A4, so there’s no significant interaction. However, both drugs can stress the liver, so long-term use should be monitored with liver function tests, especially if you have existing liver issues.
Is lopinavir/ritonavir still used for HIV today?
Yes, but only in specific situations. In high-income countries, it’s rarely used for new patients because of better-tolerated options like dolutegravir. In low- and middle-income countries, it’s still common due to cost and availability. The WHO lists it as essential, but its role is shrinking as cheaper, safer alternatives become accessible.
Why is ritonavir used in such a low dose?
Ritonavir is used at 100mg-far below the dose needed to treat HIV-because its only job is to block CYP3A4. At this low dose, it inhibits the enzyme enough to boost lopinavir without causing severe side effects like nausea or liver damage that come with higher doses. It’s a pharmacokinetic tool, not an antiviral in this context.
Can I drink alcohol while taking lopinavir/ritonavir?
Moderate alcohol is not strictly forbidden, but it’s strongly discouraged. Both alcohol and lopinavir/ritonavir are processed by the liver. Combining them increases the risk of liver inflammation and damage. Heavy drinking can lead to rapid liver failure, especially in people with existing hepatitis or fatty liver disease.
What should I do if I need surgery while on lopinavir/ritonavir?
Tell your surgeon and anesthesiologist you’re on lopinavir/ritonavir-no exceptions. Many common anesthetics, like midazolam and fentanyl, become dangerously potent when combined with ritonavir. Doses must be reduced by 60-80%. Delaying surgery to switch regimens may be safer than risking overdose.
Does lopinavir/ritonavir cause weight gain?
Lopinavir/ritonavir is less associated with weight gain than newer HIV drugs like dolutegravir or bictegravir. However, it can cause fat redistribution-loss of fat in the face and limbs, and gain around the abdomen and neck. This is called lipodystrophy and is linked to long-term use of older protease inhibitors.
How long does ritonavir’s effect last after stopping?
Ritonavir’s inhibition of CYP3A4 lasts beyond its own half-life (3-5 hours). Because it permanently damages the enzyme, it takes 5-7 days for your liver to produce enough new CYP3A4 to restore normal metabolism. During this time, other drugs may still be affected. Never assume interactions stop immediately after stopping ritonavir.
What Comes Next?
If you’re on lopinavir/ritonavir and have no reason to stay on it-like access issues or cost-you should talk to your provider about switching. Newer regimens are simpler, safer, and just as effective. If you can’t switch right now, treat your medication list like a live document. Review it every time you see a new doctor, pharmacist, or specialist. Keep a printed copy of your full drug list, including doses and frequencies, and bring it to every appointment.
The goal isn’t just to treat HIV. It’s to live without constant risk of dangerous interactions. Lopinavir/ritonavir does its job-but at a high cost. Knowing how to manage that cost is the real skill.






Comments
rachna jafri
They don't want you to know this but ritonavir isn't just boosting lopinavir-it's part of a global pharmaceutical cartel designed to keep people dependent on complex, expensive regimens. The WHO? Controlled. The FDA? Compromised. Look at how they pushed Paxlovid during COVID-same damn trick. They want you to believe it's science when it's really profit-driven mind control. And don't get me started on how they're phasing out lopinavir in the West while dumping it in the Global South like a toxic legacy. It's colonial medicine with a white coat.
darnell hunter
While the pharmacokinetic interactions described are clinically significant, the assertion that ritonavir's mechanism-based inactivation of CYP3A4 constitutes a "chemical tug-of-war" is metaphorically imprecise and undermines the scientific rigor of the exposition. The enzyme's irreversible inhibition is a well-characterized biochemical phenomenon, not a narrative device. Furthermore, the comparison between cobicistat and ritonavir lacks statistical context regarding the magnitude of interaction differences, rendering the conclusion regarding "exponentially harder to manage" unsubstantiated.
Hannah Machiorlete
Okay but like… why does it feel like every time I take something for my back pain, my doctor looks at me like I just asked to borrow a kidney? I’m on this combo and I swear half the meds I’ve been prescribed since 2020 came with a 12-page warning label. I’m not even gonna ask about the statins. My liver is a warzone and I’m just trying to sleep through the night without my heart stopping.
Bette Rivas
It’s important to emphasize that while ritonavir’s dual role as both inhibitor and inducer creates a complex interaction profile, the clinical implications are not uniformly negative. For example, in patients with hepatitis C co-infection, ritonavir’s induction of CYP2C9 can reduce the plasma concentration of certain antivirals, necessitating dose adjustments-but this same property has been leveraged in research settings to study metabolic plasticity. The key is not avoidance, but precision: understanding which enzymes are affected, which drugs are substrates, and when to monitor. The Liverpool database is indispensable, but clinicians must also integrate pharmacogenomic data-particularly for CYP3A5 expressers, who may require up to 30% higher lopinavir doses. This isn’t just about safety; it’s about personalized pharmacology.
prasad gali
Let’s be clear: lopinavir/ritonavir is a relic of 2005-era HIV management. The CYP3A4 inhibition profile is a pharmacokinetic nightmare, and the drug interaction burden exceeds 1,200 entries-a liability in any modern clinical setting. The fact that it persists in LMICs is not a triumph of accessibility but a failure of global health equity. Newer regimens reduce pill burden, eliminate food restrictions, and avoid the GI toxicity profile that leads to non-adherence. If you’re still prescribing this, you’re not practicing medicine-you’re practicing archivism.
Jeff Moeller
It’s not about the drug it’s about the system that makes us need it in the first place
Why do we keep building medicines that break other medicines
Why do we treat the body like a machine that needs constant tuning
What if the real cure was less chemistry and more care
Ashley Miller
Of course they say it’s safer now. Just like they said cigarettes were safe in the 50s. They’ll tell you dolutegravir is the future while quietly stockpiling ritonavir for the next pandemic. You think they’re phasing this out? Nah. They’re just hiding it behind a new brand name and calling it "innovation." Wake up. The same people who made you believe this was necessary are the ones who control the patents, the labs, and the guidelines. They don’t want you to know how simple it could be.
Lauren Hale
I’ve worked with patients on lopinavir/ritonavir for over a decade, and the most important thing I’ve learned is this: the biggest risk isn’t the drug-it’s the silence. Patients don’t tell their dentists, their physical therapists, their ER doctors. They’re scared they’ll be judged, or worse, told to stop their HIV meds. That’s why I always give them a laminated card with their full regimen, a list of absolute no-gos (fentanyl, midazolam, rivaroxaban), and the Liverpool link. I make them read it aloud to me. If they can explain why they can’t take ibuprofen long-term without checking, they’re ready. Knowledge is the only real shield here.
Greg Knight
If you’re on this combo, I get it. It’s overwhelming. But here’s the good news-you’re not alone, and you’re not doomed. The fact that you’re reading this means you’re already doing better than most. Start small: write down every single thing you take, even the gummy vitamins. Use the Liverpool database once a week-it takes five minutes. Talk to your pharmacist, not just your doctor. They know the interactions better than anyone. And if you’re feeling overwhelmed? Take a breath. You’ve survived this long. You’re not just managing a drug regimen-you’re mastering your health. That’s power.
Paige Basford
Wait so if I take St. John’s wort for my mood and I’m on this combo, does that mean my HIV meds stop working? That’s wild. I thought herbal stuff was safe. I mean, my cousin swears by it for anxiety. So now I’m supposed to stop it and maybe get depressed just so my HIV meds work? And why isn’t this on the label? Why do I have to Google this like it’s some secret code? Feels like the system is set up to make you fail.
Ankita Sinha
This is actually one of the most eye-opening posts I’ve read in a long time. I’m from India and we still use lopinavir/ritonavir in a lot of clinics because it’s cheap and available. But I never realized how many hidden dangers it carries-like how it messes with birth control or warfarin. I’m going to share this with my local health group. We need to push for better access to dolutegravir, not just because it’s newer, but because it gives people their lives back without constant fear. Knowledge isn’t just power-it’s survival.