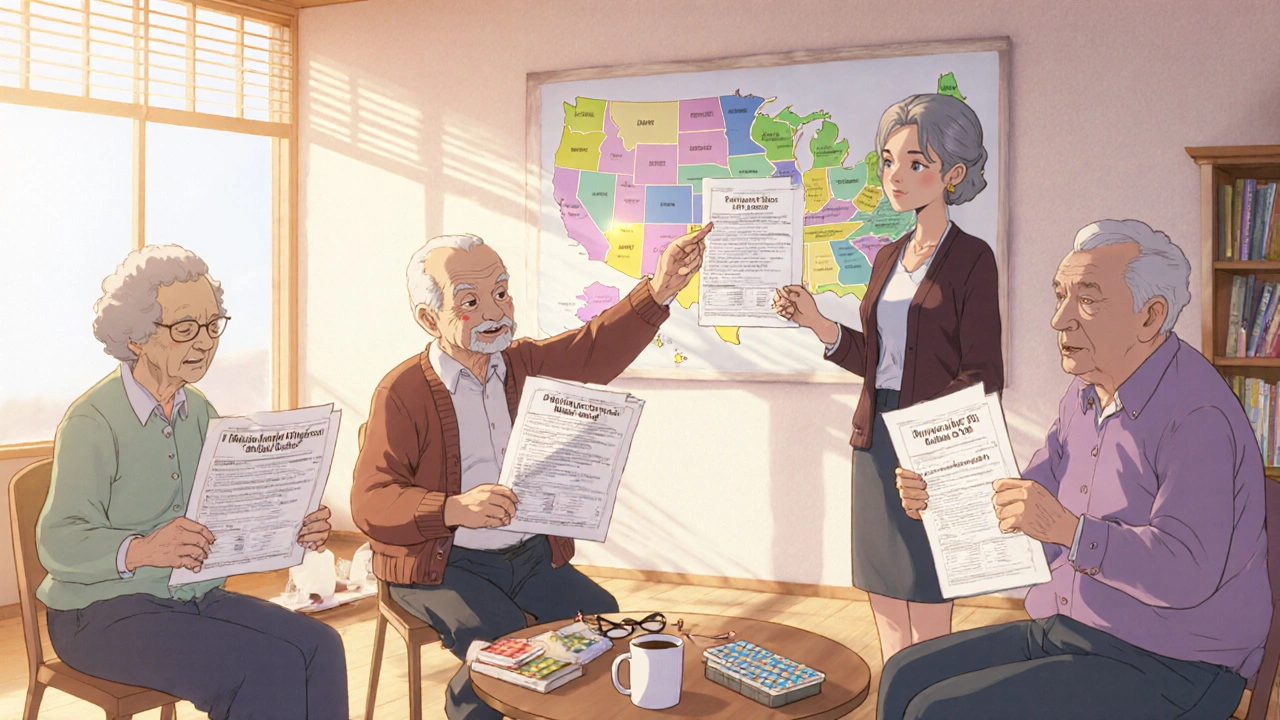
If you’re struggling to pay for prescriptions, you’re not alone. In 2025, nearly 15.2 million Americans rely on government medication assistance programs to afford their drugs. But here’s the catch: what works in New Jersey won’t necessarily help you in Texas. These programs aren’t national-they’re state-by-state, with wildly different rules, income limits, and covered drugs. Knowing which one you qualify for could save you thousands a year.
What Exactly Are State Pharmaceutical Assistance Programs (SPAPs)?
SPAPs are state-run programs designed to help people pay for prescription drugs. They’re not part of Medicare, but they often work alongside it. Most target seniors, people with disabilities, and those with low income. Some cover Part D premiums. Others pay copays or fill gaps when Medicare doesn’t cover a drug at all.
As of 2025, 32 states have active SPAPs. Their budgets range from $15 million in Wyoming to $215 million in Pennsylvania. That’s not just funding-it’s real savings for real people. For example, New Jersey’s PAAD program helped over 250,000 residents in 2024, cutting monthly drug costs by an average of $400. But if you move from New Jersey to Arizona, you lose that coverage. There’s no automatic transfer. You have to reapply from scratch.
Medicare Extra Help: The Federal Safety Net
Before you dive into state programs, check if you qualify for Medicare Extra Help. It’s a federal program run by the Social Security Administration that lowers costs for Medicare Part D. In 2025, the income limits are $23,475 for individuals and $31,725 for couples. Resource limits are $17,600 and $35,130, respectively. That includes bank accounts, stocks, and real estate (excluding your primary home).
If you qualify, you pay $0 for premiums and deductibles. Generic drugs cost $4.90 per prescription. Brand-name drugs? Just $12.15. That’s far lower than most state programs. And if you’re already on Medicaid, SSI, or a Medicare Savings Program, you get enrolled automatically.
But here’s the problem: only 42% of eligible people actually sign up. Why? The application is confusing. It takes an average of 8.5 hours to complete. And processing can take up to 90 days. During that time, you might have to pay full price for heart meds, insulin, or cancer drugs-money you don’t have.
How State Programs Compare: Real Examples
Not all SPAPs are created equal. Let’s look at three states with very different approaches.
- New Jersey (PAAD): Established in 1967, it’s one of the oldest. You must be on Medicare Part D. PAAD pays your premium if it’s $34.70 or less per month. Copays are $5 for generics, $7 for brand names. It covers insulin, needles for MS, and over 1,200 drugs. But if your doctor prescribes something not on PAAD’s formulary, you’re stuck waiting 6-8 weeks for an appeal.
- Pennsylvania (PACE): This program covers both Part D premiums and drugs Medicare won’t pay for. Income limits are higher: $27,470 for individuals, $36,900 for couples. PACE requires you to apply for Extra Help first. Then it covers what’s left. The catch? The whole process takes about 120 days. You might go without meds for four months.
- California (Medi-Cal Rx): It doesn’t just help with cost-it helps with access. Medi-Cal Rx adds 127 specialty drugs to Medicare’s formulary, including treatments for rare diseases. But eligibility is tied to Medicaid income levels, which are lower than Extra Help’s. So if you’re just above the Medicaid cutoff, you might not qualify for anything.
There’s no standard. One state pays premiums. Another pays copays. A third covers drugs Medicare ignores. And none of them tell you what to do if you move.
Why So Many People Miss Out
A 2024 study by the Medicare Rights Center found that 63% of people who moved between states experienced a coverage gap. That means they went without meds while waiting for new paperwork to clear. And it’s not just relocation. Many seniors don’t know they qualify. Others can’t navigate the forms. One Reddit user wrote: “I applied for Extra Help in March. Paid $872 out of pocket for my heart meds while I waited.”
Even when people apply, they get denied for small mistakes. A $500 gift card from a grandchild? That counts as a resource. A joint bank account with a child? That might disqualify you. The rules are written for lawyers, not retirees.
Dr. Aaron Kesselheim from Harvard put it bluntly: “The complexity of these programs creates barriers for the very people they’re meant to help.”
What’s Changing in 2025
This year brought big changes. The Inflation Reduction Act capped out-of-pocket drug costs at $2,000 annually for Medicare Part D beneficiaries. That’s down from $7,050. If you’re on Extra Help, you hit that cap faster-and your drugs become free after that.
Also, dual-eligible beneficiaries (those on both Medicare and Medicaid) can now change their drug plan once a month instead of once a year. That’s huge. If your new insulin isn’t covered, you can switch plans without waiting.
And CMS is working on a new standardized Extra Help form, launching in January 2026. The goal? Cut processing time by 30% and boost enrollment by 15%. But until then, you’re stuck with the current system.

How to Apply and What You Need
Here’s how to start:
- Check Extra Help eligibility. Go to SSA.gov or call 1-800-772-1213. You can apply online with your Social Security number, income proof (tax return or pay stubs), and asset info.
- Call your State Health Insurance Assistance Program (SHIP). Every state has free counselors-14,000 of them. They’ll help you fill out forms, understand your options, and even call your pharmacy to check coverage. Find yours at shiptacenter.org.
- Apply for your state’s SPAP. Each state has its own form. New Jersey uses the PAAD-1. Pennsylvania uses the PACE application. Don’t guess-get the right form.
- Keep copies of everything. Save your application, receipts, denial letters. If you’re denied, you can appeal.
Most programs require annual re-certification. That means every year, you’ll need to prove your income and assets again. Set a calendar reminder. Miss it, and your coverage stops.
What to Do If You’re Denied
Denials happen. Maybe your income is $50 over the limit. Maybe your bank balance was misreported. Don’t give up.
First, request a written explanation. Then, file an appeal. Most states allow you to submit updated documents-like a recent pay stub showing lower income. SHIP counselors can help with this too. In New Jersey, appeals take 30-45 days. In Pennsylvania, it can take 60.
And if you’re still stuck? Look at nonprofit groups. Organizations like NeedyMeds and Patient Access Network Foundation offer grants for specific drugs. They don’t replace government help-but they can bridge the gap.
Final Reality Check
These programs work-but only if you use them. The average beneficiary saves $4,000-$5,000 a year on drugs. That’s a mortgage payment. A car repair. A month’s rent.
But the system is broken. It’s fragmented. It’s slow. And it’s changing fast. States like California, Texas, and Florida are expanding SPAPs to cover more specialty drugs. But 7 states are projected to face funding shortfalls by 2026.
Don’t wait until you can’t afford your insulin. Don’t assume Medicare covers everything. Don’t think you’re not eligible because you own a car or have a small savings account. Check. Call. Ask. You might be surprised.
Can I get help with my prescription drugs if I’m not on Medicare?
Yes, but your options are limited. Most state pharmaceutical assistance programs (SPAPs) require you to be on Medicare Part D. However, some states offer separate programs for low-income adults under 65 who don’t qualify for Medicaid. For example, California’s CalRx program provides discounts on certain medications for uninsured residents. Check your state’s health department website or call SHIP for local options.
What if my doctor prescribes a drug not covered by my state program?
You’ll need to file an appeal. Most SPAPs have a formulary-a list of covered drugs. If your medication isn’t on it, your doctor can submit a medical exception request. This usually requires a letter explaining why the drug is medically necessary. Processing times vary: New Jersey takes 6-8 weeks, while Pennsylvania may respond in 30 days. In the meantime, ask your pharmacist about patient assistance programs from drug manufacturers.
Do I have to reapply every year?
Yes. Most state programs require annual re-certification to confirm your income and assets haven’t changed. Medicare Extra Help also requires renewal, though it’s often automatic if you’re on Medicaid or SSI. Missing the deadline means your benefits stop. Set a reminder for the same month each year. Some states mail reminders, but don’t rely on them.
Can I qualify for both Extra Help and my state’s SPAP?
Absolutely-and you should. Extra Help covers premiums and copays for Medicare Part D. Your state program often fills the gaps: paying for drugs Medicare excludes, covering higher copays, or helping with non-formulary medications. Pennsylvania’s PACE program requires you to apply for Extra Help first, then covers what’s left. In New Jersey, PAAD pays your Part D premium if it’s under $34.70. Together, they can cut your drug costs by over 80%.
Why are drug prices still high even with these programs?
Because the programs don’t control drug prices-they just help you pay for them. Specialty drugs, like those for cancer or rare diseases, are rising 12.3% per year. State budgets are only growing 4-6%. So while your copay might stay at $7, the drug’s list price could double. That’s why programs are adding more appeals, limiting coverage, or pushing patients toward cheaper alternatives. The system is under strain.
Is there help if I live in a state without a SPAP?
Yes. Even if your state doesn’t have a SPAP, you can still get Extra Help. You can also use nonprofit organizations like NeedyMeds, RxAssist, or the Patient Advocate Foundation. These groups connect you to drug manufacturer coupons, free medication programs, and grants for specific conditions. Some pharmacies, like CVS and Walgreens, offer discount cards for common drugs. Always ask your pharmacist-they know what’s available.





Comments
Julia Strothers
This is all a scam. The government doesn't care if you live or die-they just want you to stay dependent. PAAD? PACE? They’re just Trojan horses for Medicare expansion. Watch how soon they start requiring biometric scans to get insulin. And don’t get me started on the 127 ‘specialty drugs’ California added-those are all made by Big Pharma lobbyists. They’re not helping you. They’re locking you in.
Next thing you know, your Social Security number gets flagged if you buy a second car. You think that $500 gift card from Grandma is a problem? Wait till they start tracking your Amazon purchases for ‘luxury spending.’
Erika Sta. Maria
so like... if u r not on medicare u r basically f***ed? like why even have programs if they only help ppl who already have the system’s stamp of approval? its like a buffet where u need a golden ticket just to get in the door. and then they charge u for the napkins. also, why do they call it 'extra help' when it feels like extra paperwork? i applied for a library card once and it was faster.
also, is it just me or does everyone in america have to be a lawyer to survive? i live in india and we just... get medicine. sometimes. with luck. but at least we dont fill out 17 forms to buy a pill.
ps: i think the word 'formulary' is just a fancy way of saying 'we dont like your drug'
Nikhil Purohit
Hey, I’ve been helping my mom navigate this mess for the past year. The SHIP counselors are actually lifesavers-no joke. One lady in our county spent 45 minutes on the phone with us, walked us through every line of the PACE form, and even called the pharmacy to confirm coverage before we submitted.
Don’t let the bureaucracy scare you. It’s broken, yeah, but there are real people behind the systems trying to help. Just don’t wait until your insulin runs out. Start now. Call SHIP. Print out the forms. Bring a friend. You’re not alone in this.
And yes, reapplying every year sucks. But set a Google Calendar alert. Do it. Your future self will thank you.
Logan Romine
So let me get this straight… the government caps your out-of-pocket at $2,000… but only after you’ve already paid $7,000 in the first place? 🤡
And we call this ‘reform’? It’s like giving someone a parachute after they’ve already hit the ground.
Also, ‘dual-eligible’ can change plans monthly now? Cool. So now you’re a drug plan roulette champion. Congrats. You win… more paperwork. 🎰💊
Meanwhile, my cousin’s insulin went up 40% this year. The ‘help’ is just a really expensive distraction.
Chris Vere
The structure of pharmaceutical assistance reveals a deeper truth about modern governance: it is designed to manage scarcity rather than eliminate it. The state programs, though fragmented, are not failures-they are adaptations to a system that prioritizes administrative control over human dignity.
One must ask: why must eligibility be tied to income thresholds that change annually? Why must the sick become accountants to survive? The answer lies not in policy, but in power. The complexity is intentional. It filters out the desperate. Only the persistent survive.
Yet still, we persist. For that, we are not victims. We are witnesses.
Noah Fitzsimmons
Oh wow, you actually think people don’t know about this? Please. Everyone who’s ever had a kid on insulin knows this system is rigged. But the real joke? The people who wrote this post think they’re being helpful by listing programs. Nah. You’re just handing out life rafts while the Titanic’s band plays on.
And don’t get me started on ‘patient assistance programs.’ Those are just corporate PR stunts. Pfizer gives you a coupon for $10 off a $1,200 drug. That’s not help. That’s a slap in the face with a receipt.
Also, ‘set a calendar reminder’? You think I’m gonna remember to reapply when I’m too tired to shower because I’m spending my paycheck on metformin? Get real.
Eliza Oakes
Okay but why does California get to cover 127 specialty drugs and Texas just says ‘lol good luck’? Is this a competition? Who’s winning? California? Congrats. You’re the only state that pretends to care.
Also, I applied for Extra Help last year. Got denied because my bank account had $1,701. Not $1,700. Not $1,699. $1,701. So I had to pay $1,400 for my blood thinner. That’s not a mistake. That’s a trap.
And now I’m supposed to ‘appeal’? With what? My tears? My receipts? My dignity? I’m done. I’m just gonna stop taking half my meds and hope I die quietly. #MedicareIsAMinefield
Clifford Temple
Foreigners don’t get it. This isn’t about ‘access’-this is about sovereignty. America’s programs are OURS. We built them. We fund them. And now we’re being told to beg for insulin like we’re in some third-world country? No.
These programs are under attack by globalists who want to replace them with a one-size-fits-all UN healthcare plan. That’s why they make the forms so confusing. So you give up. So you turn to ‘international aid.’
Don’t fall for it. Fight for your state program. Call your rep. Demand more funding. Don’t let them take this away.
And if you’re not a U.S. citizen? Then maybe you should focus on your own country’s problems before lecturing us on Medicare.
Corra Hathaway
Y’all are making this way harder than it needs to be 😤
Here’s the truth: YOU ARE WORTHY of help. Even if you’re over the income limit by $50. Even if you have a car. Even if you have $2k in savings. That’s not ‘luxury.’ That’s survival.
Call SHIP. Again. And again. And again. They don’t mind. They want you to succeed. I had a counselor cry with me when I got approved. That’s not a robot. That’s a human who chose this job because they care.
And if you get denied? Appeal. Send a handwritten letter. Include a photo of your pill organizer. Make them see you. You’re not a case number. You’re a person.
I’m rooting for you. 💪❤️
Shawn Sakura
Just a quick note: I applied for PAAD last year. Took 11 weeks. Got denied. Sent in corrected tax forms. Got approved on the second try. Took 3 more weeks. I’m now saving $387/month on my heart meds. It’s not perfect. But it’s real.
Also, the typo in my application? I wrote ‘$23,475’ as ‘$23,477.’ They didn’t care. They called me. Asked if I meant $23,475. I said yes. They fixed it. No penalty. No drama.
So yeah, the system is broken. But it’s not broken for everyone. You just have to keep showing up. And if you’re tired? That’s okay. Just keep going. One step. One form. One phone call. You’ve got this.
Swati Jain
Let’s deconstruct the formulary paradigm: SPAPs operate within a neoliberal framework that commodifies health outcomes. The formulary is not a clinical tool-it’s a gatekeeping mechanism designed to optimize cost containment over therapeutic efficacy.
When New Jersey delays appeals for 6-8 weeks, they’re not being inefficient-they’re performing structural violence. The system is engineered to induce attrition. The goal is not to help. The goal is to reduce enrollment.
And yet… I still applied. Because resistance, even in bureaucratic form, is still resistance. 🧠
David vaughan
Just wanted to say thank you for this post. I didn’t know about SHIP. I called mine today. The counselor helped me get Extra Help approved in 3 days. I’m crying. Not because I’m sad. Because for the first time in 18 months… I can breathe.
You don’t have to do this alone. Seriously. Call them. They’re waiting.
Shawn Sakura
Just read your comment, David. I’m Shawn-the guy who wrote the one above. You’re not alone. I called SHIP again today because my mom’s meds changed. They helped us switch to a better plan. I cried too.
It’s messy. It’s slow. But it’s worth it. Keep going. We’re all in this together.