Imagine rolling over in bed and suddenly the room spins. You grab the headboard, feel nauseous, and wonder if you’re having a stroke. This isn’t rare. In fact, BPPV is the most common cause of vertigo you’ve never heard of. It’s not a brain tumor. It’s not a stroke. It’s not even a mystery. It’s loose crystals in your inner ear - tiny calcium pieces called otoconia - that got stuck where they don’t belong. And there’s a simple, proven fix.
What Exactly Is BPPV?
BPPV stands for Benign Paroxysmal Positional Vertigo. Let’s break that down. Benign means it’s not dangerous. Paroxysmal means it comes in sudden bursts. Positional means your head position triggers it. And vertigo is that spinning sensation, even when you’re perfectly still.
Every time you move your head - rolling over, looking up at a shelf, bending down to tie your shoes - the loose crystals in your inner ear shift. They’re supposed to sit in the utricle, helping you sense gravity. But when they break loose, they float into the semicircular canals. These canals are filled with fluid and lined with hair cells that detect movement. When the crystals bump into them, they send false signals: “You’re spinning!” - even though you’re just turning your head.
It’s not a brain problem. It’s not a nerve issue. It’s a mechanical glitch. And that’s why most treatments don’t involve pills.
Who Gets BPPV - And Why?
BPPV hits people over 50 most often. About 1 in 20 adults will get it at some point. Women are 1.5 to 2 times more likely than men. Why? No one’s sure, but it may be linked to hormonal changes, bone density, or even minor head trauma you don’t even remember - like bumping your head on a cabinet or falling off a step stool years ago.
It’s also more common if you’ve had a head injury, inner ear infection, or prolonged bed rest. People with osteoporosis or vitamin D deficiency have higher rates, too. In fact, one study showed taking 1,000 IU of vitamin D daily cut recurrence by nearly a quarter.
But here’s the thing: in over half of cases, there’s no clear cause. It just happens. And that’s why so many people get misdiagnosed.
Why Doctors Miss It - And What You Should Know
Most people with BPPV see their doctor, get a CT scan or MRI, and are told, “It’s probably just stress.” That’s because BPPV doesn’t show up on imaging. The only way to diagnose it is by watching your eyes move - specifically, by doing the Dix-Hallpike test.
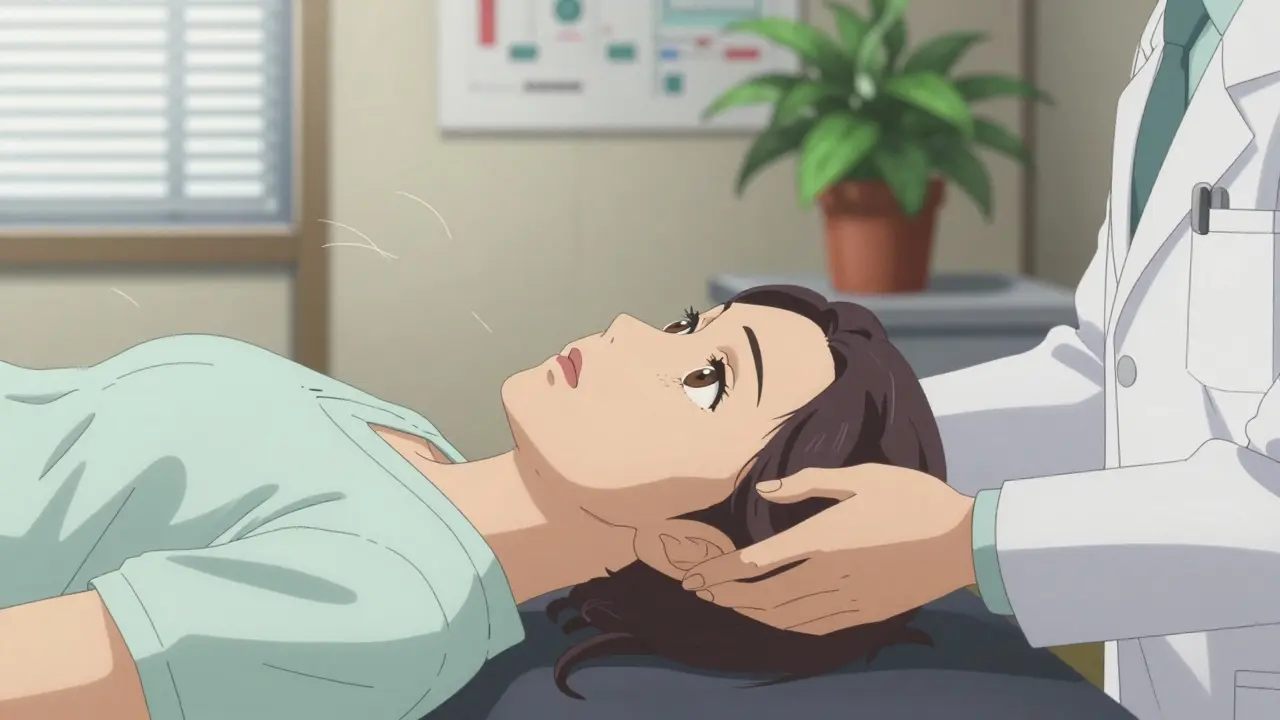
Here’s how it works: your doctor sits you up, then quickly lowers you onto your back with your head hanging off the edge of the table and turned to one side. If you have BPPV in your right posterior canal, your eyes will jerk upward and twist - a telltale sign called torsional nystagmus. And it won’t start right away. There’s a 2- to 10-second delay. Then it fades. That’s called latency and fatigability. These are the hallmarks of BPPV.
Compare that to a stroke, which causes constant dizziness, slurred speech, weakness, or double vision. Or Meniere’s disease, which includes ringing in the ears and hearing loss. BPPV doesn’t affect hearing. It doesn’t cause numbness. It’s purely about head position.
And yet, 35% of primary care doctors misdiagnose it. Why? Because they weren’t trained to do the test. Or they’re scared of missing something serious. But the truth? MRI has less than a 5% chance of finding anything useful in a classic BPPV case. And it costs $1,200-$1,800 extra.

Canalith Repositioning: The Real Cure
Here’s the good news: BPPV can be fixed in minutes - no surgery, no drugs, no hospital stay.
The treatment is called canalith repositioning. It’s a series of controlled head movements designed to guide the loose crystals back into the utricle, where they belong. The most common version is the Epley maneuver.
It goes like this:
- You sit upright on a table, with your legs extended.
- The doctor turns your head 45 degrees to the side that triggers your dizziness.
- They quickly lay you back, keeping your head turned and hanging slightly off the table.
- You stay there for 30-60 seconds until the spinning stops.
- They turn your head 90 degrees to the opposite side - still lying down.
- After another 30 seconds, they roll you onto your side, facing the floor.
- Finally, they help you sit up, keeping your head slightly bent forward.
That’s it. One session. Takes less than five minutes. And it works 80-90% of the time for posterior canal BPPV - which is 80-90% of all cases.
There are other versions too. The Semont maneuver is faster but more jerky. The Lempert roll is used when the crystals are in the horizontal canal. Each one is tailored to where the crystals are stuck.
And here’s the kicker: you can do the Epley maneuver at home. Video-guided apps and YouTube tutorials show people getting relief in their own living rooms. One study found home-based Epley maneuvers worked 72% of the time when done with video instructions - compared to just 45% with written steps.
What Doesn’t Work - And Why
Most people are offered medication first. Meclizine. Dramamine. Benzodiazepines. These are vestibular suppressants. They numb the inner ear signals. They make you drowsy. They don’t fix the problem.
Studies show these drugs are only 18% effective for BPPV. And they don’t prevent recurrence. In fact, they can delay real treatment. Patients often take them for weeks, feeling worse, while the crystals keep floating around.
Same goes for balance exercises like Brandt-Daroff. They can help - but they take two weeks of doing 20 reps twice a day. That’s 280 movements. And even then, only about half the people get full relief. Compare that to the Epley maneuver: one session, one-time fix.
And don’t waste money on expensive vestibular rehab equipment unless you have complex, recurring cases. For most people, the Epley maneuver - done right - is all you need.

What Happens After Treatment?
Most people feel better immediately. Some feel a little off for a day or two - like they’re on a boat. That’s normal. Your brain is relearning what’s real.
But BPPV loves to come back. About 15% of people get it again in a year. By five years, it’s 35%. By ten years, half of all patients will have another episode.
That doesn’t mean you’re broken. It just means your inner ear is prone to losing crystals. Some people get it every few years. Others get it once and never again.
There’s no way to prevent it completely. But staying active, avoiding prolonged bed rest, and checking your vitamin D levels can help. One study showed people with low vitamin D had higher recurrence rates - and supplementing cut it by 24%.
And if it comes back? Do the Epley maneuver again. Or go back to your doctor. There’s no shame in it. It’s not a failure. It’s just how the body works.
When to Worry - And When Not To
BPPV is not dangerous. But vertigo can be a sign of something serious. Here’s when to get urgent help:
- Vertigo that lasts longer than a minute
- Weakness in your arms or legs
- Slurred speech or trouble swallowing
- Double vision or sudden vision loss
- Severe headache with no known cause
- Loss of consciousness
If you have any of these, go to the ER. They could be signs of stroke or a brain tumor.
But if your dizziness only happens when you roll over, look up, or bend down - and it lasts less than a minute - you’ve got BPPV. And it’s fixable.
Real People, Real Results
On Reddit’s r/Vertigo community, over 12,000 people share stories. One man, 68, said he hadn’t slept on his side in three years because of vertigo. After one Epley maneuver, he slept through the night for the first time in years.
A teacher in Texas said she couldn’t bend over to help her students without getting dizzy. She did the maneuver at her doctor’s office. By lunchtime, she was picking up books again.
And a nurse in Bristol - just like me - told me she kept getting dizzy when she turned her head to check on patients. She thought it was stress. Her ENT did the Dix-Hallpike test in five minutes. She did the Epley maneuver that day. No more spinning. No more meds. No more fear.
This isn’t magic. It’s science. And it’s available to anyone who knows to ask for it.
Is BPPV the same as general dizziness?
No. General dizziness is vague - lightheadedness, unsteadiness, feeling faint. BPPV is specific: a sudden spinning sensation triggered by head movement, lasting less than a minute. It’s not about blood pressure or anxiety. It’s about crystals in your inner ear.
Can I do the Epley maneuver on myself?
Yes - if you know which ear is affected. Use a video guide or app like DizzyFix. If you’re unsure, see a provider first. Doing it on the wrong side won’t help and might make symptoms worse temporarily. Most people feel better after one try, but it’s best to confirm the diagnosis before self-treating.
Why do I still feel off after the Epley maneuver?
It’s normal. Your brain has been getting false signals for days or weeks. Even after the crystals are back in place, your brain needs time to recalibrate. You might feel slightly unsteady for 24-48 hours. Avoid sudden head movements during that time. If dizziness returns after a few days, you may need another session.
Do I need an MRI for BPPV?
No - unless you have red flags like weakness, numbness, or speech problems. BPPV doesn’t show up on MRI. The diagnosis is made by history and the Dix-Hallpike test. Unnecessary imaging adds cost and delays treatment. The American Academy of Otolaryngology recommends against routine scans for typical BPPV cases.
Can BPPV cause hearing loss?
No. BPPV affects the semicircular canals, not the cochlea - the part of the ear responsible for hearing. If you have hearing loss, ringing, or fullness in your ear along with dizziness, you may have Meniere’s disease or another condition. See an ENT for proper testing.
How many times do I need the Epley maneuver?
Most people feel better after one session. About 1 in 3 need a second or third try, especially if the crystals are stubborn or stuck in multiple canals. If symptoms persist after three attempts, your provider should check for other causes - like vestibular neuritis or a different type of BPPV.
If you’ve been told your dizziness is “just aging” or “stress,” don’t accept that. Ask for the Dix-Hallpike test. Ask about the Epley maneuver. You don’t need to live with spinning. There’s a fix - and it’s simple.






Comments
Shane McGriff
I used to think vertigo was just stress-until I did the Dix-Hallpike and my doctor confirmed it was BPPV. I’d been avoiding sleeping on my side for two years. One Epley maneuver, and I slept through the night for the first time since my 50th birthday. No meds. No scans. Just a 5-minute fix. Why do doctors still skip this test? It’s insane.
And yeah, vitamin D? I started taking 1000 IU daily after reading this. Been 8 months. No recurrence. Small change, huge difference.
Jacob Cathro
LMAO so we’re just supposed to believe some ‘crystals’ in your ear are spinning you out? Like… what, they’re tiny disco balls? Next they’ll say your brain’s got a glitchy Spotify playlist.
And don’t even get me started on ‘home Epley’-you think some guy on YouTube knows more than an MD? I’ve seen people do it wrong and end up with vertigo in THREE canals. Classic case of internet medicine.
Also-vita D? Bro, you’re telling me my dizziness was because I didn’t take a gummy? What’s next? Cinnamon for cancer?
kumar kc
Stop wasting time with pills. Do the maneuver. Simple.
Medicine is broken when people need a blog post to learn basic anatomy.
Thomas Varner
Okay, but… has anyone else noticed how weird it is that the Epley maneuver works so well… but only if you do it exactly right? Like, one degree off, and it’s useless?
I tried it at home after watching three videos. Did it three times. First time, I got dizzy for 20 minutes. Second time, I felt like I was in a washing machine. Third time… boom. No spinning.
So… it’s not magic. It’s physics. And my brain is just… bad at trusting gravity now.
Also, I did it after eating a burrito. Bad idea. Don’t do that.
And yes, I’m still scared to roll over. I’ve been sleeping in a chair for a week. Worth it.
Arlene Mathison
THIS. This is the kind of post that saves lives. I’ve been telling my friends for years: if you get dizzy when you roll over, don’t just take meclizine and hope it goes away. Ask for the Dix-Hallpike. Seriously. It takes five minutes.
I had BPPV after my knee surgery-I was bedridden for 10 days. When I finally got up, boom-spinning every time I looked up. My PT did the maneuver. I cried. Not from pain. From relief.
And vitamin D? I got mine checked. Was at 22. Now I’m at 58. No more dizziness. No more fear. You’re not broken. You’re just missing a little sunshine.
Share this. Please. Someone you love is suffering right now and thinking it’s ‘just aging.’
Emily Leigh
So… you’re telling me the entire medical system is built on fear… and this one tiny, stupid head movement is the cure?
And we pay $1500 for an MRI… but the real fix is a YouTube video?
I’m not mad… I’m just… disappointed. Like, we’re this close to a revolution in medicine and we’re still stuck in the ‘let’s scan everything’ era.
Also-why do I feel like I’m being gaslit by my own inner ear?
…I’m gonna do the Epley right now. Wish me luck. Or send memes. Either works.
Carolyn Rose Meszaros
OMG YES 😭 I did the Epley at home with the DizzyFix app and it worked on the first try. I’ve been avoiding my own bed for 14 months. Now I’m sleeping on my side again. I cried. I hugged my cat. I posted this on Facebook.
Also-vita D? My doctor said I was ‘borderline.’ Took 1000 IU daily. Three months later, my BPPV didn’t come back. I’m not a scientist. I’m just a person who stopped being scared.
Thank you for writing this. You’re a hero. 🙏💖
Nadia Watson
It is of paramount importance to emphasize that the pathophysiology of benign paroxysmal positional vertigo is not adequately understood by the general public, and consequently, misdiagnosis remains alarmingly prevalent within primary care settings.
While the Epley maneuver demonstrates statistically significant efficacy in repositioning otoconial debris, it is imperative that clinicians be formally trained in the Dix-Hallpike diagnostic protocol, as improper execution may lead to iatrogenic complications.
Furthermore, while vitamin D supplementation may correlate with reduced recurrence rates, causation has not been definitively established, and thus, recommendations should be made with caution.
Nonetheless, the dissemination of accurate, evidence-based information such as this is a vital step toward patient empowerment and improved clinical outcomes.
-Nadia Watson, MD, PhD, Department of Neuro-Otology, Johns Hopkins
Courtney Carra
What if… the crystals aren’t the problem? What if they’re just the symptom?
What if BPPV isn’t about loose calcium… but about the soul losing its balance?
We live in a world that spins too fast. We’re always looking up, always turning, always rushing. Maybe the ear doesn’t need fixing… maybe we do.
…I did the Epley anyway. It worked.
But I still think there’s something deeper here.
And I’m not just saying that to sound profound. I’m serious.
…also, I did it while listening to Enya. It helped.