When Your Body Stops Talking to Itself
You stand up from the couch. The room spins. Your vision goes gray. You barely make it to the chair before you’re dizzy, nauseous, and sweating. This isn’t just being lightheaded. It’s your autonomic nervous system failing - the part of your body that runs everything without you thinking about it: your heart, your gut, your blood pressure, your sweat glands. When nerves in this system get damaged - a condition called autonomic neuropathy - your body starts to shut down in ways that feel random, terrifying, and deeply misunderstood.
Most people with autonomic neuropathy have diabetes. About 85% of cases come from years of high blood sugar eating away at tiny nerves. But it can also happen after viral infections, chemotherapy, or autoimmune diseases. The damage doesn’t show up on a regular MRI or blood test. It hides in how your body responds - or doesn’t respond - to simple things like standing up or eating a meal.
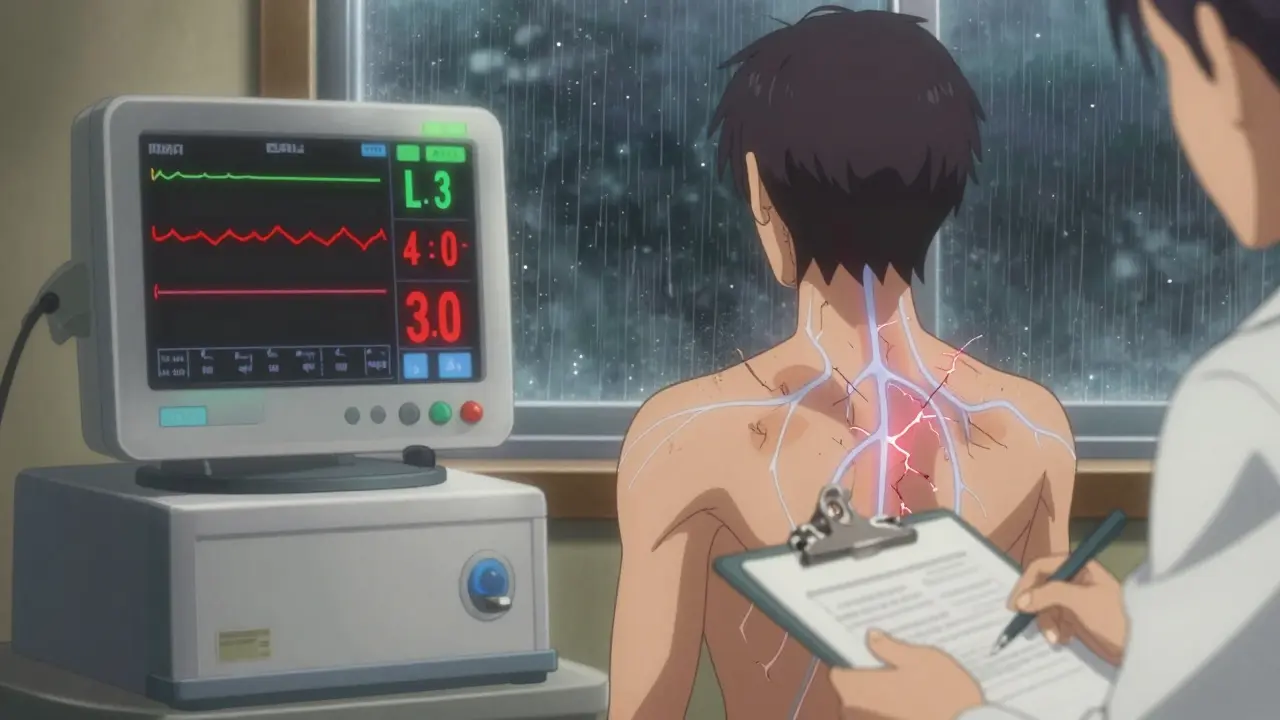
Why You Feel Like You’re Falling When You Stand Up
When you stand, gravity pulls blood down into your legs. A healthy body reacts instantly: blood vessels tighten, heart rate speeds up slightly, and blood pressure stays steady. In autonomic neuropathy, that reflex breaks. The nerves that tell your blood vessels to squeeze don’t get the message. So your blood pressure plummets.
This is called orthostatic hypotension. It’s not just a quick dizzy spell. It’s a drop of 20 mmHg or more in systolic pressure - sometimes 35 mmHg or higher - within three minutes of standing. In severe cases, people report their blood pressure falling from 120/80 to 85/55 in under 30 seconds. That’s not normal. That’s your body losing control.
Up to 30% of people with diabetic autonomic neuropathy experience this. And it’s not just about fainting. Many live with near-constant presyncope - that sick, wobbly feeling before you pass out. One study found 42% of patients had these episodes at least once a week. They avoid standing too long. They sit down after showering. They wear compression socks just to get through the day.
Some people develop POTS - Postural Orthostatic Tachycardia Syndrome - instead. Their blood pressure doesn’t drop much, but their heart races. Over 120 beats per minute when standing. Their chest feels tight. Their head pounds. They can’t walk to the kitchen without needing to sit down. POTS is often misdiagnosed as anxiety. But it’s a measurable autonomic failure - and it’s real.
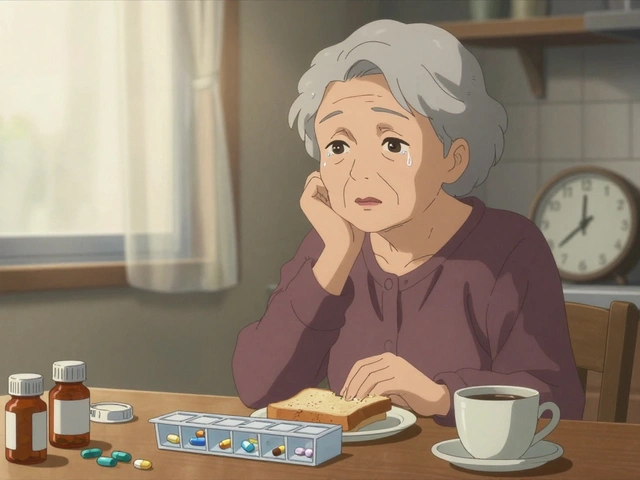
Your Gut Isn’t Broken - It’s Nerve-Damaged
Now imagine eating breakfast. You finish your toast. An hour later, you’re bloated. Two hours later, you’re vomiting. Three hours later, you still feel full. Your stomach hasn’t moved. This isn’t indigestion. It’s gastroparesis - a direct result of autonomic nerve damage.
Up to 30% of people with diabetic autonomic neuropathy develop gastroparesis. The stomach muscles stop contracting properly. Food sits there, rotting, fermenting. Scintigraphy tests - where you swallow a radioactive meal - show more than 10% of food still in the stomach after four hours. That’s abnormal. That’s disease.
And it’s not just delayed emptying. Many people get alternating constipation and diarrhea. The nerves that control bowel movement are damaged too. Constipation hits 60% of patients - some going only once or twice a week. Diarrhea? That’s often caused by bacterial overgrowth in the small intestine. When food sits too long, bacteria feast on it and release gas, toxins, and fluids. One study found 52% of autonomic neuropathy patients with GI symptoms had this condition, compared to just 15% of healthy people.
Swallowing becomes hard. Food gets stuck. Esophageal motility tests show weak, uncoordinated contractions. People avoid bread, meat, raw veggies. They eat six tiny meals a day. They stop going out to eat. Social life fades. One patient wrote: “I used to love Sunday brunch. Now I eat oatmeal in bed and pretend I’m fine.”
How Doctors Miss It - And How to Get Diagnosed
Most doctors don’t look for autonomic neuropathy unless you’re already in crisis. A 2021 audit found primary care physicians recognized symptoms in only 30% of cases. Patients wait an average of 4.7 years for a correct diagnosis. They see gastroenterologists, cardiologists, neurologists - all treating pieces of the puzzle, not the whole disease.
Here’s what actually works for diagnosis:
- Active stand test: You stand for 10 minutes while your blood pressure and heart rate are monitored. A drop of 20 mmHg systolic or 10 mmHg diastolic confirms orthostatic hypotension.
- Heart rate variability: You breathe deeply for a minute. A ratio of exhale-to-inhale heart rate below 1.1 means your autonomic system isn’t adjusting properly.
- Valsalva maneuver: You blow hard into a tube for 10 seconds. A healthy body shows a clear rise and fall in blood pressure. In autonomic neuropathy, it’s flatlined.
- Gastric emptying scan: You eat a meal with a tiny bit of radioactive tracer. A camera tracks how fast it leaves your stomach. Over 10% retention at 4 hours = gastroparesis.
- COMPASS-31 questionnaire: A 31-question survey that scores autonomic symptoms from 0 to 100. Above 30? You have significant dysfunction.
These aren’t fancy tests. They’re simple, low-cost, and widely available. Yet they’re rarely ordered unless you specifically ask. If you have diabetes and feel dizzy when standing or nauseous after eating, say: “I think I might have autonomic neuropathy. Can we check?”

What Actually Helps - Not Just the Drugs
There’s no cure. But there are ways to live better.
For blood pressure drops:
- Compression stockings (30-40 mmHg) reduce symptoms by 35%. They squeeze your legs, pushing blood back up.
- Abdominal compression garments help too - they stabilize your gut and reduce blood pooling.
- Increasing salt and fluid intake - up to 2.5 liters of water and 8-10 grams of salt daily - boosts blood volume. It’s not a joke. It works.
- Midodrine (2.5-10 mg three times a day) tightens blood vessels. It helps 70% of people - but you can’t take it before bed. It causes dangerous high blood pressure when lying down.
- Fludrocortisone makes your body hold onto salt and water. It helps 60%, but 35% end up with high blood pressure while lying down.
For gastroparesis and GI issues:
- Diet changes are the most effective long-term fix. Eat six small meals a day. Avoid fat over 25g and fiber over 10g per meal. Cook veggies until soft. Skip carbonation. No raw salads. One study showed this cut vomiting episodes by half.
- Pyridostigmine (30-60 mg three times daily) improves nerve signaling in the gut. It helps 55% of patients with minimal side effects - and no black box warning.
- Erythromycin can help short-term - but most people build tolerance in 2-4 weeks.
- Metoclopramide is risky. After 12 weeks, it can cause permanent movement disorders. Many doctors won’t prescribe it anymore.
- Ivabradine (5-7.5 mg twice daily) slows heart rate in POTS. It doesn’t fix blood pressure, but it stops the racing. 65% of patients report better quality of life.
And yes - some people get relief from fecal microbiota transplants. Early trials show 40% improvement in GI symptoms. It’s experimental, but promising.
The Real Cost of Being Invisible
Autonomic neuropathy doesn’t kill you quickly. But it steals your life slowly.
People with severe cases live 8.2 years less than those with diabetes alone. They can’t work. They can’t travel. They can’t eat out. They cancel plans because they’re afraid of passing out in public. One Reddit user wrote: “I had to quit my job because I couldn’t stand at the register without blacking out. My boss thought I was lazy.”
And the loneliness? It’s crushing. No one understands why you can’t just “push through.” Why you need to lie down after showering. Why you eat applesauce for dinner. Why you carry a water bottle and salt packets everywhere.
But you’re not alone. Over 1.5 million Americans have this. Many more are undiagnosed. The American Diabetes Association will soon recommend screening for everyone with over 7 years of diabetes. That’s progress.
What you need now isn’t a miracle. It’s recognition. It’s a doctor who listens. It’s a treatment plan that doesn’t just mask symptoms - but helps you live with them.
Your body didn’t fail. Your nerves did. And that’s something we can fix - slowly, carefully, and with real results.





Comments
Solomon Ahonsi
This is the most overblown pile of medical jargon I've seen in weeks. People just need to drink more water and stop being lazy. Stop making excuses for your body giving up.
George Firican
There's something profoundly tragic about a body that forgets how to regulate itself - like a symphony where half the instruments have gone mute, and the conductor is nowhere to be found. Autonomic neuropathy isn't just a medical condition; it's the silent unraveling of an internal ecosystem that once ran with perfect, invisible grace. We treat symptoms like bugs in a machine, but what if the machine is mourning its own broken wiring?
Matt W
I’ve lived with this for 12 years. The compression socks, the salt packets, the 6 meals a day - it’s all real. No one gets it until they’re the one collapsing after a shower. Thanks for writing this. You just described my life.
Akhona Myeki
In South Africa, we do not have access to these expensive diagnostic tests. You people in the West treat nerve damage like a luxury problem. We treat diabetes with insulin and prayer. Your 31-question survey is a joke when people are dying from lack of basic care.
Sandeep Kumar
Diabetes causes this so why are you acting like its some rare mystery. Its basic biology. If you eat sugar for 10 years your nerves rot. End of story. Stop overcomplicating
Vatsal Srivastava
POTS is just anxiety with a fancy name. All these studies are funded by pharma to sell more drugs. You don't need a gastric emptying scan. Just stop being so sensitive
Brittany Marioni
I just want to say - thank you. This is so important. So many people are suffering in silence, and this post validates their experience with such care and precision. Please keep sharing. You’re helping people feel seen. 💛
Nick Flake
I cried reading this. Not because it was sad - but because for the first time, someone put into words the invisible war I’ve been fighting. The vomiting after toast. The 3 p.m. blackouts. The shame of carrying salt packets like a secret weapon. This isn’t just medicine. It’s survival. And you just gave me a battle cry. 🫡
Bob Hynes
Man this post hit different. I got this from chemo and honestly thought I was just getting old. Turns out my gut’s been on vacation for 5 years. Compression socks are a game changer. Also, I just started eating mashed potatoes for every meal. No regrets.
Eli Kiseop
I had no idea gastroparesis was this common. I thought I was just bad at digestion. So many people are suffering and no one talks about it. Why is this not in med school curriculum
Ellie Norris
Just wanted to add - if you’re on fludrocortisone and lying down with a headache, you might be holding too much fluid. Try reducing salt for a few days and see if it helps. Also, I always spell ‘gastroparesis’ wrong. Sorry.