What Is Multiple System Atrophy?
Multiple System Atrophy is a rare, progressive brain disorder that damages nerve cells controlling movement, balance, and automatic body functions like blood pressure and bladder control. It’s not Parkinson’s disease, even though the symptoms can look similar at first. MSA affects about 0.6 to 0.7 people per 100,000 each year-far less common than Parkinson’s, which impacts roughly 1 million Americans. Most people start showing symptoms between 50 and 60, with the average age of onset at 54. Men are slightly more likely to develop it than women.
There are two main types: MSA-P (parkinsonian type) and MSA-C (cerebellar type). About 65-70% of cases are MSA-P, where movement problems like slowness and stiffness dominate. The rest are MSA-C, where balance and coordination issues are more obvious. Both types share one critical feature: widespread nerve cell death in areas of the brain that control movement and autonomic functions. The hallmark sign under the microscope is clumps of a protein called alpha-synuclein inside support cells in the brain-something that also happens in Parkinson’s, but in different patterns and locations.
How MSA-P Differs From Parkinson’s Disease
At first glance, MSA-P can look a lot like Parkinson’s. People have slow movements, stiff muscles, trouble with balance, and sometimes tremors. But the differences are sharp-and they matter a lot.
People with Parkinson’s usually have a resting tremor-a shake when their hands are still. In MSA-P, tremors are more likely to happen when holding a position, like reaching for a cup, and they’re often jerky, not rhythmic. About 60% of MSA-P patients get tremors, but they’re not the classic Parkinson’s tremor. The face often becomes expressionless, speech gets soft and quivery, and swallowing becomes harder. Many lose the ability to chew properly or speak clearly.
The biggest clue that it’s not Parkinson’s? Levodopa. This drug helps most Parkinson’s patients move better. But in MSA-P, only 15-30% get any real benefit-and even then, it lasts maybe a year or two before it stops working. If someone’s symptoms don’t improve after trying a high dose of levodopa for six months, MSA should be strongly suspected.
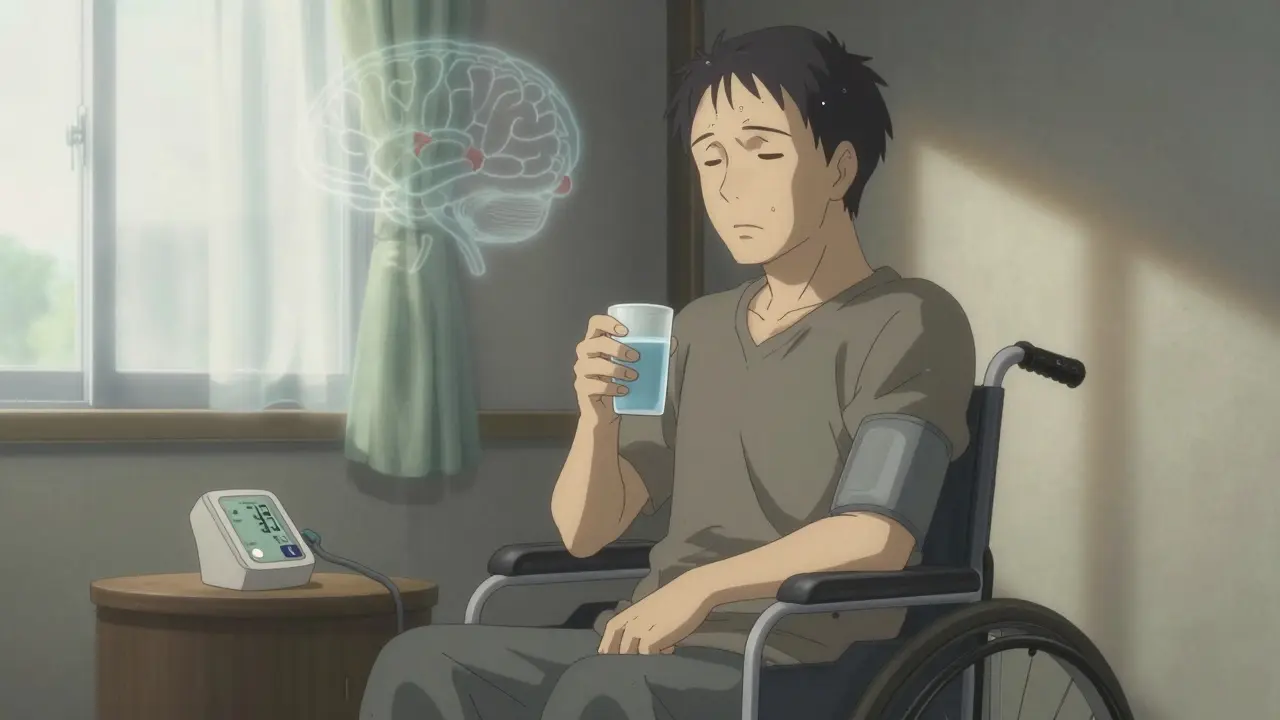
Another major difference? The speed of decline. Parkinson’s can progress slowly over decades. MSA-P doesn’t wait. Within five years of symptoms starting, half of MSA-P patients have lost most of their motor function. By 3.5 years, most need a cane or walker. By 5.3 years, they’re in a wheelchair. That’s not slow aging-it’s rapid neurological collapse.
Autonomic Dysfunction: The Silent Killer
What really sets MSA apart isn’t just the movement problems-it’s the body’s internal systems shutting down. Autonomic dysfunction isn’t a side effect in MSA. It’s a core feature, and often the first sign.
Orthostatic hypotension-dramatic drops in blood pressure when standing-is present in 90% of MSA patients. This isn’t just feeling lightheaded. It’s fainting, falling, and sometimes hitting the ground hard enough to break bones. Many people report their first symptom was blacking out when getting up from the toilet or the couch.
Bladder problems hit 85-90% of patients. Urgency, frequency, incontinence-these aren’t just annoying. They’re constant, life-limiting. Men face near-universal erectile dysfunction, often years before any movement issues appear. Sleep isn’t restful either. Eighty to ninety percent have REM sleep behavior disorder, acting out violent dreams, kicking, yelling, even jumping out of bed. Sleep apnea is common too, making nights exhausting and days even worse.
Temperature control fails. Some lose the ability to sweat in parts of their body, leading to overheating. Others can’t regulate body heat at all. These aren’t minor quirks. They’re signs the brainstem-the control center for automatic functions-is dying.

Prognosis: Why MSA-P Is So Devastating
The prognosis for MSA-P is grim. Median survival from symptom onset is only 6 to 10 years. Five years after diagnosis, 52-68% of patients are still alive. By ten years, that number drops to just 9-23%. That’s not a slow decline-it’s a race against time.
MSA-P progresses faster than MSA-C. Patients with the parkinsonian type reach the point of being bedridden in about 5.7 years, compared to 8.3 years for those with the cerebellar type. The poor response to levodopa is a bad sign. Those who don’t respond at all live an average of 6.2 years. Those who get some benefit live about 9.8 years-still a short time.
Death usually comes from complications: respiratory infections (45%), sudden cardiac events (20%), or aspiration pneumonia from swallowing problems (15%). Many patients choke on food or saliva because their brain no longer controls the reflexes that keep airways clear. Once that happens, it’s often a downward spiral.
Quality of life plummets fast. A 2021 survey of 327 MSA patients found that 78% rated their quality of life as poor or very poor within four years of diagnosis. Compare that to Parkinson’s, where only 35% feel that way at the same stage. The difference isn’t just medical-it’s emotional, social, and financial.
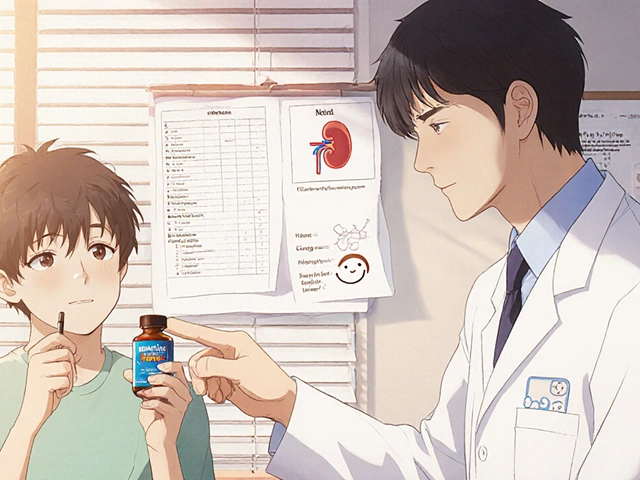
How Doctors Diagnose MSA
There’s no single blood test or scan that confirms MSA. Diagnosis is based on symptoms, timing, and ruling out other conditions. The key is recognizing patterns.
Early autonomic failure-like fainting or bladder issues-within the first three years of movement problems is the strongest indicator. If someone has balance trouble and can’t stand without help, and their blood pressure crashes when they sit up, MSA is likely. MRI scans can show telltale signs: the "hot cross bun" pattern in the brainstem (seen in 50-80% of MSA-C cases) or shrinkage of the putamen (a brain region involved in movement).
By the time symptoms are clear enough for an 85-90% accurate diagnosis, it’s often been 3 to 5 years since the first sign. That’s too late for any current treatment to stop the damage. Researchers are now working on biomarkers-like measuring neurofilament light chain in blood (which rises 3-5 times higher in MSA than normal)-to catch the disease earlier. A large study expected to finish in 2024 aims to get diagnostic accuracy above 90% within one year of symptoms starting.

Current Treatments: Managing Symptoms, Not the Disease
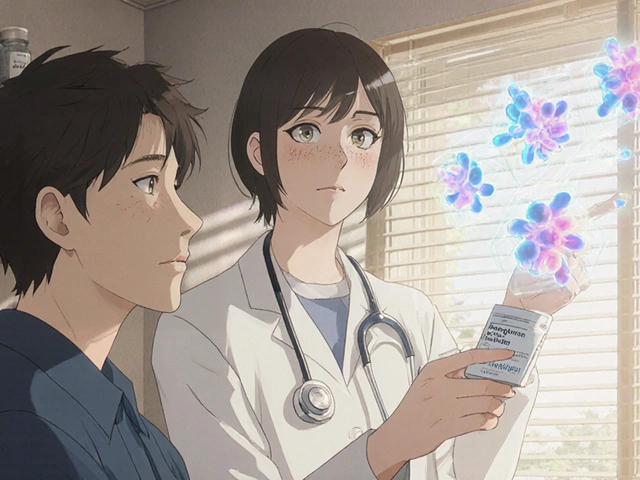
There is no cure. No drug stops MSA from progressing. Treatment is about keeping people as comfortable and safe as possible for as long as possible.
For low blood pressure, doctors use fludrocortisone, midodrine, or droxidopa-drugs that help tighten blood vessels and raise pressure. These can reduce fainting, but they don’t fix the root problem. For bladder issues, catheters, anticholinergics, or botox injections help. For sleep disorders, melatonin or clonazepam may reduce dream-acting behaviors.
Levodopa is still tried, even though most won’t benefit. High doses (up to 1,000 mg daily) are used for 3-6 months to see if there’s any response. If not, it’s stopped to avoid side effects like nausea or confusion.
Physical therapy helps maintain mobility as long as possible. Speech therapy tackles swallowing and voice problems. Urologists manage bladder issues. Nutritional support becomes critical when chewing and swallowing fail. A feeding tube may be needed later on.
There’s been hope for drugs targeting alpha-synuclein, the protein that clumps in MSA brains. Trials like PASADENA showed only a tiny 1.2-point slowing on a symptom scale over 18 months-barely meaningful. As of late 2023, only three clinical trials worldwide are testing disease-modifying therapies. Progress is painfully slow.
What the Future Holds
Right now, MSA research is stuck. We know what’s happening in the brain, but not why. We know how fast it kills, but not how to stop it. The most urgent need, according to leading researchers, is early diagnosis. By the time movement problems appear, 50-70% of the affected neurons are already gone.
Teams in Europe and the U.S. are building diagnostic tools that combine blood tests, MRI scans, and autonomic function tests to catch MSA earlier. If we can identify it within a year of the first symptom, we might finally have a chance to slow it down.
But until then, the reality remains harsh. MSA-P doesn’t give people time. It doesn’t respond to hope. It doesn’t care about good intentions. It just takes.
For families, the hardest part isn’t the medical facts-it’s the speed. One patient on a support forum wrote: "My neurologist said most people with MSA-P don’t live beyond 8 years from diagnosis. I’m 55. That’s not a prognosis. That’s a countdown."
Is Multiple System Atrophy the same as Parkinson’s disease?
No. While both cause movement problems like stiffness and slowness, MSA is a distinct disease. It affects more areas of the brain, causes severe autonomic failure early on, and responds poorly to levodopa. Parkinson’s usually progresses slowly over decades; MSA-P often leads to wheelchair use within five years.
Can MSA be cured?
No. There is currently no cure for MSA. Treatments focus on managing symptoms like low blood pressure, bladder problems, and movement issues. No drug has been shown to stop or reverse the nerve damage.
How long do people live after being diagnosed with MSA-P?
The median survival time is 6 to 10 years from when symptoms first appear. About half of patients live 5 years or more, but only 9-23% survive 10 years. Progression is faster than in Parkinson’s disease, and death often results from pneumonia, respiratory failure, or sudden cardiac events.
Why does MSA cause fainting?
MSA damages the brainstem areas that control blood pressure. When standing, the body can’t tighten blood vessels quickly enough, causing a sudden drop in pressure-called orthostatic hypotension. This leads to dizziness, lightheadedness, and fainting. It affects 90% of MSA patients and often appears early in the disease.
Are there any new treatments on the horizon?
Research is focused on early diagnosis and stopping alpha-synuclein buildup. Blood tests measuring neurofilament light chain and advanced MRI scans are being tested to detect MSA within a year of symptom onset. Clinical trials for drugs targeting the disease process are limited and so far have shown minimal benefit. The biggest breakthrough needed is earlier detection.




Comments
Eli Kiseop
So MSA isn't just Parkinson's with extra steps? I always thought the tremors were the big tell but apparently it's the whole body shutting down like a bad laptop
My uncle had something like this and they kept saying 'Parkinson's' until he couldn't stand up without help and then it was too late. Why don't they test for this sooner?
clarissa sulio
This is why we need better funding for American neuroscience. Other countries are wasting money on fringe research while our own people are dying from something we could diagnose if we just cared enough.
Monica Slypig
Look i dont even know why we bother with these rare diseases when we got real problems like obesity and gun violence
Also the fact that they say 'men are slightly more likely' but then dont say why is so typical of academic elitism
They just want grant money not answers
Becky M.
My mom’s neurologist mentioned MSA once but we didn’t know what it meant until it was too late
It’s heartbreaking how fast it goes
I wish more doctors would just say ‘this might be MSA’ earlier instead of waiting for the ‘hot cross bun’ sign
People deserve to know what they’re fighting before they’re stuck in a wheelchair
jay patel
Let me tell you something about MSA and why no one talks about it properly
It’s not just the brainstem dying it’s the entire system of care collapsing around the patient
Doctors don’t get trained on this, insurance won’t cover the right scans, families are left googling at 3am while their loved one chokes on their own saliva
And then we get some researcher in a lab coat saying ‘we need earlier detection’ like that’s a revelation
We’ve known this for 20 years
The problem isn’t the science it’s the indifference
And yes I’ve been there
My cousin lasted 4 years and the hospital didn’t even have a speech therapist on staff
That’s not medical failure
That’s societal failure
Ansley Mayson
Another rare disease post. Everyone acts like this is new news.
It’s been 30 years since the first papers. We’ve had the same stats since the 90s.
Why are we still surprised?
Dan Pearson
Oh wow MSA is just Parkinson’s but worse and faster and no one cares? Shocking.
Let me guess the drug companies are too busy selling $100,000 cancer drugs to fix this?
And of course the FDA won’t approve anything until someone dies in a clinical trial
Meanwhile real people are choking on their breakfast while some guy in a lab in Switzerland runs a 5-year study on alpha-synuclein
Can we just give people morphine and call it a day?
Akhona Myeki
While I appreciate the clinical detail, I must respectfully assert that the Western medical paradigm’s fixation on neurodegenerative biomarkers neglects the holistic interplay between environmental toxicity, nutritional deficiencies, and epigenetic expression-factors that are systematically underrepresented in current diagnostic frameworks, particularly in non-Western populations where access to advanced neuroimaging remains prohibitively limited.