Every year, thousands of older adults end up in emergency rooms because they took two pills that did the same thing-without knowing it. It’s not a mistake you can afford to make. If you’re 65 or older and see multiple specialists, you’re at high risk for duplicate medications. One doctor prescribes a blood pressure pill. Another, unaware, prescribes another one. Both lower your blood pressure. Together, they might drop it too far. You get dizzy. You fall. You’re rushed to the hospital. This isn’t rare. It’s common. And it’s preventable.
Why Specialists Don’t Know What Other Doctors Prescribed
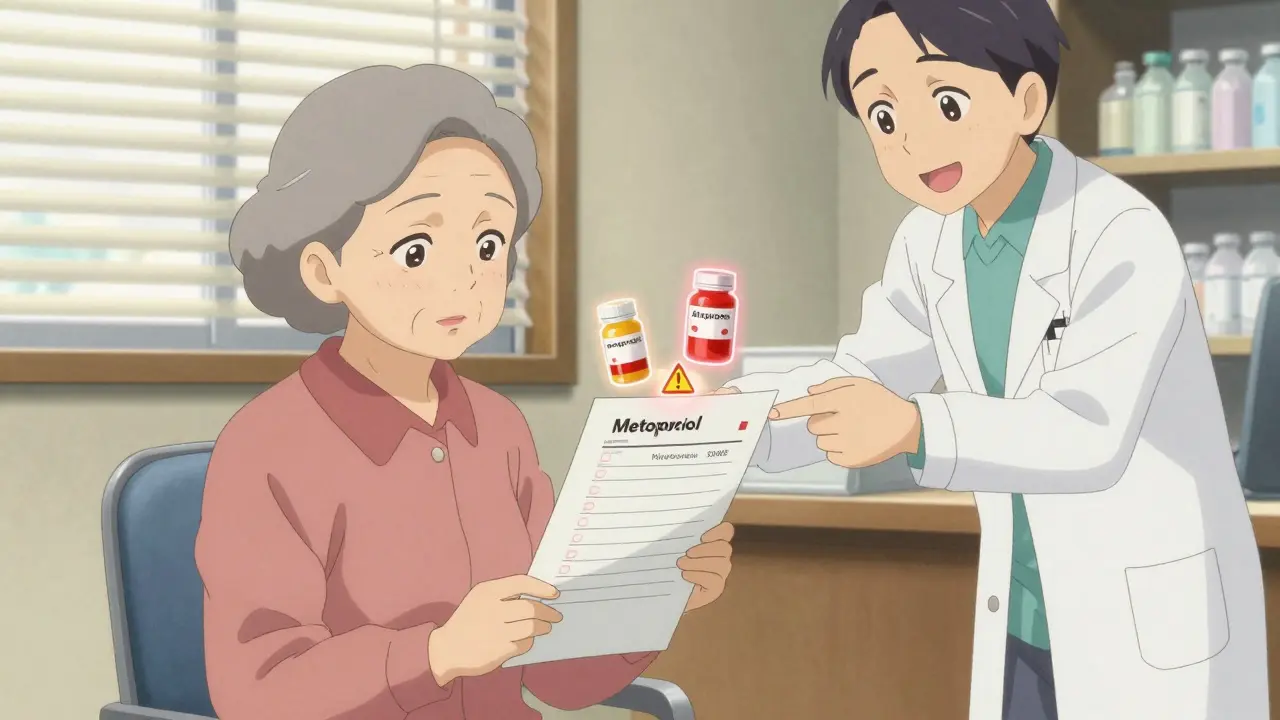
Specialists focus on one part of your body. A cardiologist treats your heart. An endocrinologist handles your thyroid or diabetes. A neurologist deals with your nerves. They’re not trained to be your full-picture pharmacist. They see your lab results, your symptoms, your latest test. But they rarely see your full list of meds unless you bring it. Even when they use electronic records, many systems don’t show prescriptions from other clinics. If your primary care doctor is in a different network than your cardiologist, their systems might not talk. And even if they do, alerts often get ignored. A 2015 study found that pharmacists spotted duplicate prescriptions in 32% of cases-but doctors overrode the warning 40% of the time. Why? Too many alerts. Too little time. Too much noise. The result? You end up with two drugs from the same class. Maybe two beta-blockers for blood pressure. Two statins for cholesterol. Two NSAIDs for pain. Each one alone is safe. Together? They can cause kidney damage, internal bleeding, or dangerously low heart rate.What Counts as a Duplicate Medication
A duplicate isn’t always the same brand name. It’s the same effect. Here are common pairs that trip people up:- Metoprolol and atenolol (both beta-blockers for heart rate and blood pressure)
- Simvastatin and atorvastatin (both statins for cholesterol)
- Omeprazole and esomeprazole (both proton pump inhibitors for acid reflux)
- Acetaminophen and combination painkillers like Percocet (which also contain acetaminophen)
- Warfarin and aspirin (both thin the blood-dangerous together)
Your Medication List: Your Lifeline
The single most powerful tool you have? A written, up-to-date list of everything you take. Not just prescriptions. Everything.- Brand and generic names
- Dosage (e.g., 10 mg, 2 tablets)
- How often you take it (e.g., once daily, every 8 hours)
- Why you take it (e.g., "for high blood pressure," "for arthritis pain")
- Over-the-counter pills (ibuprofen, melatonin, calcium)
- Vitamins and supplements (fish oil, vitamin D, herbal teas)
Use One Pharmacy-Always
Pharmacists are your secret weapon. They see every prescription you fill. They know if you’ve been prescribed two drugs that do the same thing. They’re trained to catch this. But only if they have your full record. If you use different pharmacies-Walgreens for one script, CVS for another, a mail-order service for your diabetes meds-you’re making it harder for them to help. One pharmacy has your blood pressure pills. Another has your cholesterol meds. They can’t see the full picture. And neither can you. Switch to one pharmacy. Even if it’s farther away. Even if you have to wait a few extra minutes. It’s worth it. Your pharmacist can flag duplicates before you even leave the counter. They can call your doctor. They can suggest alternatives. They’ve done it hundreds of times.
Ask the Right Questions at Every Visit
Don’t just say, "Thanks, I’ll take it." Ask these three questions:- "Why am I taking this?"
- "Is this new medicine replacing something I already take?"
- "Could this interact with anything else I’m on?"
Get a Medication Review
Many Medicare Advantage plans now offer free, one-on-one medication reviews with a pharmacist. Ask your primary care doctor or call your plan. These reviews take 30-45 minutes. The pharmacist sits with you, looks at your full list, and says: "You’re taking two drugs that do the same thing. You can stop one. Here’s why." Some clinics even have pharmacists built into the team. If your doctor’s office has a clinical pharmacist, ask to meet with them. They don’t just refill prescriptions-they optimize them. They cut out the duplicates. They reduce side effects. They save you money.What to Do If You’ve Already Been Prescribed a Duplicate
If you realize you’re taking two drugs that do the same thing-don’t stop either one on your own. That’s dangerous. Instead:- Call your primary care doctor. Say: "I think I might be on two medications that do the same thing. Can we review them?"
- Bring your list. Bring your pill bottles.
- Ask: "Which one should I keep? Which one can I stop?"

Technology Can Help-But Only If You Use It
There are apps now that let you take a photo of your pill bottle and it auto-fills your list. Some even sync with your pharmacy. Others send you reminders and flag potential duplicates. Examples include MyTherapy, Medisafe, and the free MyMedications app from the U.S. National Library of Medicine. They’re not magic. But they’re better than a crumpled piece of paper. The key? Use them. Update them. Share them.Real-Life Example: What Happens When You Don’t Act
An 81-year-old woman in Bristol was seeing her cardiologist for atrial fibrillation. He prescribed metoprolol. She’d been taking atenolol for years from her GP. Both are beta-blockers. She didn’t know. She started feeling faint. She fell twice in one week. Her family rushed her to the ER. Her blood pressure was dangerously low. Her heart rate was 42 beats per minute. It took three days to untangle. Her GP had no idea the cardiologist prescribed a new drug. The cardiologist didn’t know she was on another. The pharmacist flagged it-but she’d filled the new script at a different pharmacy. She didn’t need two. She needed one. And a better system.Final Checklist: What to Do Today
You don’t need to fix everything at once. Start here:- Write down every medication you take-today. Include vitamins and OTCs.
- Take a photo of each pill bottle.
- Choose one pharmacy and fill all your prescriptions there.
- Bring your list to your next doctor visit-even if it’s just for a flu shot.
- Ask your pharmacist: "Do I have any duplicate meds?"
- Call your primary care doctor and say: "I want a medication review. Can we schedule one?"
How do I know if I’m taking two drugs that do the same thing?
Check your list against common duplicate pairs like metoprolol/atenolol, omeprazole/esomeprazole, or simvastatin/atorvastatin. If you’re unsure, bring your full list to your pharmacist. They can scan your medications and tell you if any have overlapping effects. You can also use free apps like Medisafe or MyMedications that flag potential duplicates.
Can my specialist see what my primary doctor prescribed?
Not always. Many electronic health records don’t share data across different healthcare systems. Even if they do, specialists often don’t have time to review every prescription. That’s why you need to bring your own list. Don’t assume they know what’s already on your chart.
Should I stop a duplicate medication myself?
No. Stopping a medication suddenly-especially for blood pressure, heart, or mental health-can be dangerous. Contact your primary care doctor first. Ask them to review your list and tell you which one to keep and which one to taper off safely. Never make changes without medical guidance.
Are over-the-counter meds included in duplicate checks?
Yes. Many duplicates happen because people take ibuprofen daily for pain, then get prescribed naproxen from a specialist. Or they take Tylenol for headaches, not realizing their painkiller already contains acetaminophen. Always include OTCs, vitamins, and herbal supplements on your list.
How often should I update my medication list?
Update it every time you start, stop, or change a medication-even if it’s just a new bottle of vitamins. Keep it current. Bring the latest version to every appointment, including emergency visits. A dated list is worse than no list at all.
Is there a free service to help me review my meds?
Yes. Many Medicare Advantage plans offer free medication reviews with a pharmacist. Ask your plan or your primary care doctor. Some community pharmacies also offer free consultations. Don’t wait for a problem-get your list reviewed proactively. It’s one of the best ways to stay safe.





Comments
Sumler Luu
Been there. My mom took two blood pressure meds for months without knowing. She ended up in the ER after passing out in the kitchen. Now she keeps a printed list in her wallet and brings it to every appointment-even the dermatologist. Simple? Yes. Life-saving? Absolutely.
Fabio Raphael
I work in a clinic and see this every week. Specialists are great at their jobs, but they’re not mind readers. I’ve had patients come in with 12 meds and zero idea why they’re taking half of them. The real fix isn’t just better tech-it’s empowering patients to speak up. Ask the questions. Bring the list. Don’t wait for someone else to catch it.
Rajni Jain
omg this is so real!! my dad took two diff pain meds and ended up with a bleeding ulcer 😭 he didn’t even know tylenol was in his other pill. now we use medisafe and it sends alerts. also, we switched to one pharmacy and it’s been a game changer. pharmacists are unsung heroes 🙏
Natasha Sandra
THIS. 👏 I’ve been yelling this from the rooftops since my grandma almost died from a duplicate statin. 🚨 Stop trusting doctors to know everything. You are your own best advocate. Print it. Photo it. Text it to your kids. Use emojis if you have to. 💊📱❤️
Erwin Asilom
The systemic failure here is not individual negligence-it’s fragmented healthcare infrastructure. Electronic health record interoperability remains a national scandal. While patient education is critical, the burden should not rest solely on the elderly. Policy reform must prioritize seamless data exchange between providers and pharmacies.
Sophia Daniels
Oh honey, you think this is bad? Wait till you see what happens when someone takes a blood thinner and then gets a NSAID from their ‘wellness coach’ at the yoga studio. 🤦♀️ We’re letting people die because we’re too lazy to make systems talk. And don’t even get me started on how Medicare refuses to fund pharmacist consultations unless you’re on hospice. This isn’t an accident. It’s negligence dressed up as bureaucracy.
Steven Destiny
Listen. If you’re over 65 and seeing more than one specialist, you’re already at risk. This isn’t scary-it’s simple. One pharmacy. One list. Three questions. Do it today. Your future self will hug you. And if you’re too busy? Tell your kid. Or your neighbor. Or your mailman. Someone needs to do this for you. Don’t wait for the fall.
Amy Lesleighter (Wales)
my aunt took two acid reflux pills and her kidneys gave out. she didn’t know omeprazole and esomeprazole were the same thing. now she uses a free app. it’s not fancy. it’s just a photo of her bottles. but it saved her. you don’t need to be smart. you just need to be consistent. write it down. even if it’s messy.
Becky Baker
Why do we even have this problem? Because we let foreign companies run our pharmacies and tech systems. If we had American-made EHRs and American pharmacists who actually talked to each other, this wouldn’t happen. Stop outsourcing your health to corporations that don’t care if you live or die.
sakshi nagpal
As someone from India where polypharmacy is rampant due to unregulated OTC sales, I can say this issue transcends borders. In my village, elders take 10+ pills daily because ‘the doctor said so’-no one checks interactions. The solution isn’t just tech-it’s community. Train local health workers to help families maintain lists. Make it a cultural norm to ask: ‘What’s this for?’ We must normalize vigilance, not silence. This post is a lifeline.