Every year, thousands of older adults in the UK and beyond are told they need to take a blood thinner to prevent a stroke - but then they hesitate. Why? Because they’ve fallen before. Or their child has. Or their neighbour broke a hip after a tumble and ended up in the hospital. The fear is real: anticoagulants can turn a simple fall into a life-threatening bleed. But what if not taking them is even riskier?
Why Seniors Need Anticoagulants
Atrial fibrillation (AFib) affects nearly 1 in 10 people over 65. It’s not just an irregular heartbeat - it’s a silent threat. In AFib, blood pools in the heart and can clot. If that clot travels to the brain, it causes a stroke. The risk doesn’t creep up slowly. It spikes. At age 70-79, the chance of a stroke in a year jumps to nearly 10%. By 80-89, it’s over 23%. That’s more than 1 in 5 people. Warfarin, used since the 1950s, cuts that risk by two-thirds. Newer drugs - apixaban, rivaroxaban, dabigatran, edoxaban - do the same or better. They don’t need weekly blood tests like warfarin. They’re easier to take. And for seniors, that matters. A 2015 study of over 800 people aged 85-89 found they got the most benefit from anticoagulants. Not less. More.The Fall Fear: Real, But Misplaced
It’s true: seniors on blood thinners who fall are more likely to bleed badly. A Minnesota hospital study showed that 90% of fall-related deaths involved people over 85 or on anticoagulants. That statistic haunts families. It haunts doctors too. But here’s what that number doesn’t tell you: most seniors with AFib will never fall. And of those who do, most won’t die from it. What’s far more likely? A stroke. The evidence is clear - elderly patients are far more likely to suffer a stroke than a fatal fall. In fact, the BAFTA trial, which followed 81 elderly patients (average age 81.5), found that those on anticoagulants had a 52% lower risk of stroke or systemic embolism than those on aspirin. And there was no significant increase in major bleeding. The American College of Cardiology, American Heart Association, and Heart Rhythm Society all agree: age and a history of falls are not reasons to avoid anticoagulants. In fact, they say the opposite - the older you are, the more you stand to gain.DOACs vs. Warfarin: What’s Better for Seniors?
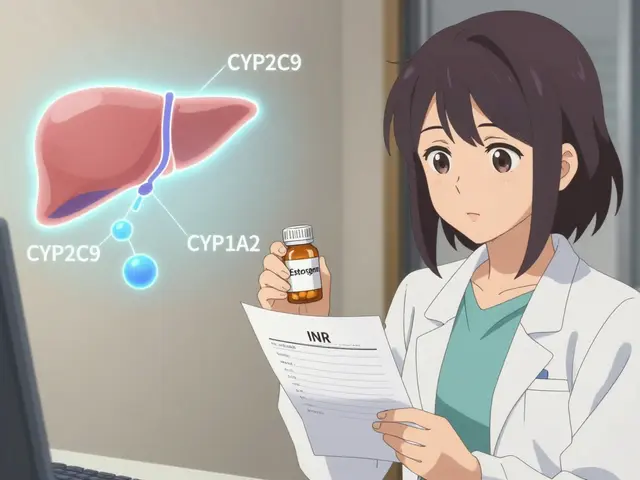
There are two main types of anticoagulants: warfarin and DOACs (direct oral anticoagulants). Warfarin works well, but it’s finicky. You need regular blood tests to make sure your INR is between 2.0 and 3.0. Many seniors struggle with that. Miss a test? The dose is off. Too high? Risk of bleeding. Too low? Risk of stroke. DOACs don’t need those tests. They’re fixed-dose. Apixaban (Eliquis) reduces stroke risk by 21% compared to warfarin - and cuts major bleeding by 31% in patients over 75. Rivaroxaban lowers the chance of brain bleeds by 34%. Edoxaban reduces major bleeding by 8.5% compared to warfarin. And dabigatran slashes stroke risk by 88% versus placebo. But DOACs have a catch: most are cleared by the kidneys. As we age, kidney function drops. That’s why doctors check creatinine clearance every 6 to 12 months. If it falls below 50 mL/min, the dose may need to be lowered. That’s not a reason to stop - it’s a reason to adjust.
Reversal Agents: What Happens If There’s a Fall?
One of the biggest worries for families is: “What if they fall and break their head? Can we stop the bleeding?” For warfarin, vitamin K and fresh frozen plasma can reverse it - but slowly. For DOACs, we now have specific reversal agents. Idarucizumab (Praxbind) reverses dabigatran within minutes. Andexanet alfa (Andexxa), approved in 2015, reverses apixaban, rivaroxaban, and edoxaban. These aren’t perfect - they’re expensive and not always available in rural clinics - but they exist. And they’ve changed the game. In a 2021 study published in Circulation, apixaban showed fewer major bleeds than warfarin in patients over 75 - even when falls happened. The safety gap widened with age.What Doctors Get Wrong - And What They Should Do Instead
A 2021 survey found that 68% of primary care doctors would refuse to prescribe anticoagulants to an 85-year-old with two falls in the past year - even if their stroke risk score (CHA2DS2-VASc) was 4, meaning they had a 10% annual stroke risk. That’s not evidence-based. That’s fear-driven. The right approach? Don’t stop anticoagulation because of falls. Instead, reduce the risk of falling. Start with a fall risk assessment: the Morse Fall Scale or a simple home safety check. Remove loose rugs. Install grab bars. Improve lighting. Review all medications - benzodiazepines, sleep aids, painkillers, even some antidepressants can make you dizzy. Then, add exercise. The Otago Exercise Program, proven in multiple studies, reduces falls by 35% in seniors. It’s simple: leg strengthening and balance training, done twice a week at home. No gym needed. And yes - use the HAS-BLED score. It includes falls, high blood pressure, kidney disease, and age. But a score over 3 doesn’t mean “don’t give anticoagulants.” It means “monitor closely.”
The Numbers Don’t Lie - But They’re Often Ignored
Only 55-60% of eligible seniors with AFib get anticoagulants. That number drops to 48% for those over 85. Meanwhile, stroke rates in this group keep climbing. The math is brutal: for every 100 octogenarians on anticoagulants for one year, 24 strokes are prevented. Three major bleeds happen. That’s a net gain of 21 prevented bad outcomes. In contrast, if you skip anticoagulation and one stroke happens? Recovery is rarely complete. Paralysis. Speech loss. Dementia. Nursing home. Death. The bleeding risk? Often treatable. Especially with newer reversal agents. And most bleeds - even serious ones - don’t lead to death.What Families Should Ask
If your parent or loved one has AFib and you’re worried about falls, ask these questions:- What’s their CHA2DS2-VASc score? Is it 2 or higher?
- Have we checked their kidney function in the last 6 months?
- Have we done a home fall risk assessment?
- Are we reviewing all their meds for dizziness or sleep aids?
- Are they doing balance exercises? Can we start the Otago program?
- What’s the plan if they fall? Do we know how to reverse the anticoagulant?
What’s Next?
New trials are underway. The ELDERLY-AF study is tracking apixaban use in people over 85. The 2024 ACC Expert Consensus Pathway recommends lower DOAC doses for seniors with mild kidney decline - not stopping them. AI tools are being tested to predict fall risk by analyzing walking patterns from smartwatches. The bottom line? Anticoagulants save lives in seniors. Not despite falls - but by managing them wisely. The goal isn’t to avoid all falls. It’s to prevent strokes. And for most older adults with AFib, that’s the real danger.Don’t let fear of falling stop you from protecting someone from a stroke that could change everything.






Comments
Lance Nickie
nah bro, if they fall they die, just let em be.
Rosalee Vanness
Look, I’ve been caring for my 87-year-old mom since she got diagnosed with AFib last year, and I’ll tell you - the fear of falls is real, but the fear of stroke? That’s a whole different kind of nightmare. We did the home safety overhaul: non-slip mats everywhere, handrails on every step, removed three rugs that looked innocent but were basically death traps. We started the Otago program - twice a week, she does squats with a chair and stands on one foot while holding the counter. She complains, but she’s more stable now. And yes, she’s on apixaban. The doctor said her CHA2DS2-VASc was 5, and her kidneys? Still above 50. We check every six months. I used to think anticoagulants were for people who didn’t have grandchildren to hug - turns out, they’re for people who want to keep hugging them. The bleeding risk? Yeah, it’s there. But so’s the risk of waking up one morning and realizing your mom can’t say your name anymore. That’s the trade-off nobody talks about until it’s too late.
John Tran
you know what’s funny? we live in a society that worships youth but treats the elderly like walking time bombs. we give them pills to slow aging, then panic when they fall - like gravity is a moral failure. anticoagulants aren’t the enemy, fear is. we’ve turned medicine into a gamble where the house always wins if you’re over 75. but here’s the truth: life isn’t about avoiding death. it’s about living so fully that death doesn’t feel like a loss - just a transition. if your grandma can still laugh at bad puns and watch her favorite soap operas without a stroke stealing her mind? that’s victory. we don’t need to protect them from falling - we need to protect them from being told they’re too old to deserve a full life. the body fails. the soul doesn’t have to.
mike swinchoski
if you let old people take blood thinners then you're just enabling them to die messily. why not just let nature take its course? they're gonna die anyway. this is just prolonging the suffering.
Lethabo Phalafala
I’m from South Africa, and in my community, we don’t just ‘manage’ elderly care - we hold it. My auntie, 83, has AFib. We didn’t just hand her a pill and walk away. We sat with her. We called the clinic. We checked her kidney function. We bought her a cane with a grip that doesn’t slip. We installed lights in the hallway. And yes - she’s on rivaroxaban. Not because we’re reckless. Because we’re brave. The WHO says 80% of strokes in elderly patients are preventable. Why are we treating anticoagulants like a last resort? They’re a lifeline. And if you’re scared of bleeding, learn how to reverse it. Don’t let ignorance be the reason someone loses their voice, their memory, their dignity. We owe our elders more than fear. We owe them action.
Milla Masliy
My mom is 81, on dabigatran. We had a long talk with her cardiologist. He said, ‘We don’t stop meds because they fall - we fix why they fall.’ So we did: PT for balance, removed the throw rug by the bathroom, switched her sleep med from lorazepam to melatonin. She fell last month - hit her head, but no bleed. The reversal agent was in the ER, just in case. She’s fine. And she’s still baking her famous apple pie. I don’t want her to live longer - I want her to live better. Anticoagulants let her do that. The data doesn’t lie. Neither does her smile.
Priyanka Kumari
As someone who works with elderly patients in rural India, I see this daily. Families say, ‘We can’t afford the tests, we can’t afford the drugs.’ But the real cost? A stroke. One stroke means losing a caregiver, losing income, losing dignity. We teach them: use the CHA2DS2-VASc score. Check creatinine. Do balance exercises - even just holding onto a chair for 30 seconds twice a day helps. DOACs are expensive here, but generics are coming. And yes - we have reversal agents now, though access is uneven. But the mindset? That’s the biggest barrier. We don’t say ‘too old.’ We say ‘let’s protect her.’ And that changes everything.
Avneet Singh
Frankly, the entire discourse is clinically reductive. The CHA2DS2-VASc and HAS-BLED scores are population-level constructs - they lack individualized phenotypic granularity. When you conflate fall history with anticoagulation contraindication, you’re engaging in heuristic-driven, algorithmic bias. The real issue is not the drug - it’s the epistemological deficit in geriatric primary care. We need longitudinal biomarker profiling, not checklists. Also, DOACs have renal clearance limitations - you’re ignoring pharmacokinetic variability in polypharmacy cohorts. This is not medicine. It’s protocol theater.
Adam Vella
It is a well-documented phenomenon that cognitive dissonance frequently manifests in geriatric care when familial anxiety overrides evidence-based guidelines. The emotional burden of potential hemorrhagic events, while understandable, is statistically disproportionate to the risk of ischemic stroke in high-risk AFib populations. The data from the BAFTA trial, the ARISTOTLE subgroup analyses, and the 2024 ACC Expert Consensus Pathway are unequivocal: advanced age is not a contraindication - it is an indication. To withhold anticoagulation on the basis of fall history is not prudent clinical judgment - it is negligence masked as caution.
Nelly Oruko
my grandma’s on eliquis. she fell. didn’t bleed. still walks her dog. stop being scared. just help.
vishnu priyanka
in my village, we say: ‘If the wind doesn’t knock you down, the silence will.’ My uncle had AFib, refused meds because he didn’t want to ‘die from a cut.’ He had a stroke. Lost half his body. Now he sits quiet. No more stories. No more chai. We gave him the drug after - but it was too late. The fall was just a shadow. The stroke was the storm. Don’t wait for the storm to teach you.
Angel Tiestos lopez
bro. i had my 88-year-old grandma on apixaban. she fell. hit her head. went to er. doc gave her andexxa. she was fine. next day she made me pancakes. 🫶. stop overthinking. she’s not a lab rat. she’s your grandma. give her the pill. fix the floor. let her live.
Alan Lin
Let me be clear: if you’re a clinician and you’re refusing anticoagulation to an elderly patient with a CHA2DS2-VASc score of 4 or higher because of a history of falls, you are not practicing medicine - you are practicing fear. You are complicit in preventable disability. The guidelines have been updated. The drugs are safer than ever. Reversal agents exist. Fall prevention is a multi-modal intervention - not a reason to withhold care. You are not protecting them. You are abandoning them. This isn’t risk-averse care. It’s care-averse negligence. And if you’re okay with that, you shouldn’t be holding a stethoscope.
Acacia Hendrix
It’s fascinating how the entire narrative hinges on a reductive binary: stroke versus bleed. But what about microbleeds? Silent cerebral hemorrhages? The cumulative burden of anticoagulant-induced microvascular injury in the aging brain? The literature on this is sparse, yet the long-term cognitive implications are underexplored. And let’s not forget the confounding effect of frailty - a non-linear, multidimensional construct that renders population-level risk scores inadequate for the very oldest. The DOACs may be ‘better,’ but they are not benign. We are treating symptoms, not pathophysiology. And until we address the neuroinflammatory cascade of aging, we’re just rearranging deck chairs on the Titanic.
Trevor Davis
Hey, I get it - I’m a nurse and I’ve seen the aftermath. One guy, 86, fell, hit his head on the tile, and bled into his skull. Scary stuff. But here’s the thing: I’ve seen way more people come in with strokes from skipping their blood thinners. One lady, 82, didn’t take hers because she was scared. Had a stroke on a Tuesday. Didn’t recognize her own daughter on Friday. She’s in a nursing home now. The blood thinner? It’s not the villain. The fear? That’s the real killer. So yeah - check the kidneys. Fix the house. Start the exercises. But don’t skip the pill. Your grandma’s memory? It’s worth it.