Warfarin Estrogen Interaction Calculator
How This Calculator Works
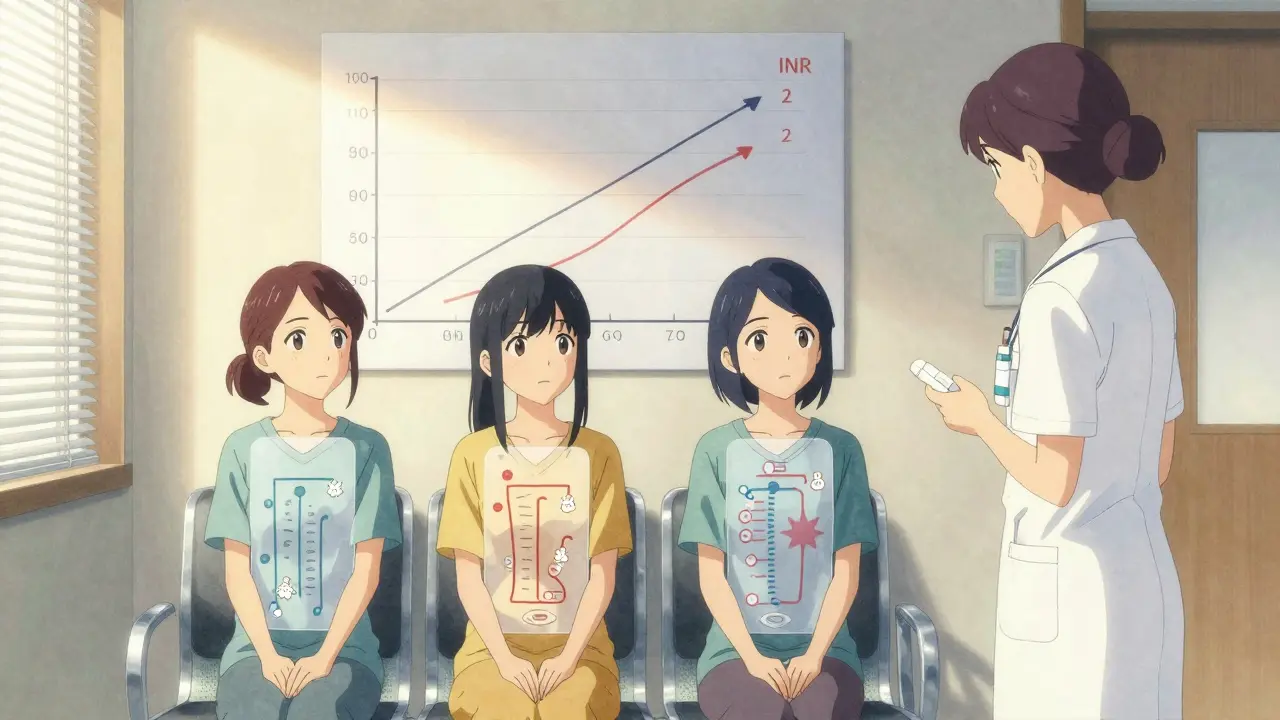
This tool helps estimate how estrogen therapy may affect your INR while on warfarin. Based on real-world data from the INR Registry and clinical studies, it shows expected INR changes and recommended warfarin adjustments.
When you're on warfarin, even small changes in your routine can shake up your blood thinner's effectiveness. Add estrogen into the mix-whether from birth control, hormone replacement therapy, or other sources-and things get even trickier. This isn't just a theoretical concern. Real people, real clinics, and real data show that estrogen can push INR levels up or down, sometimes dangerously so. And yet, many patients and even some providers don't know what to watch for.
How Estrogen Changes Warfarin's Effects
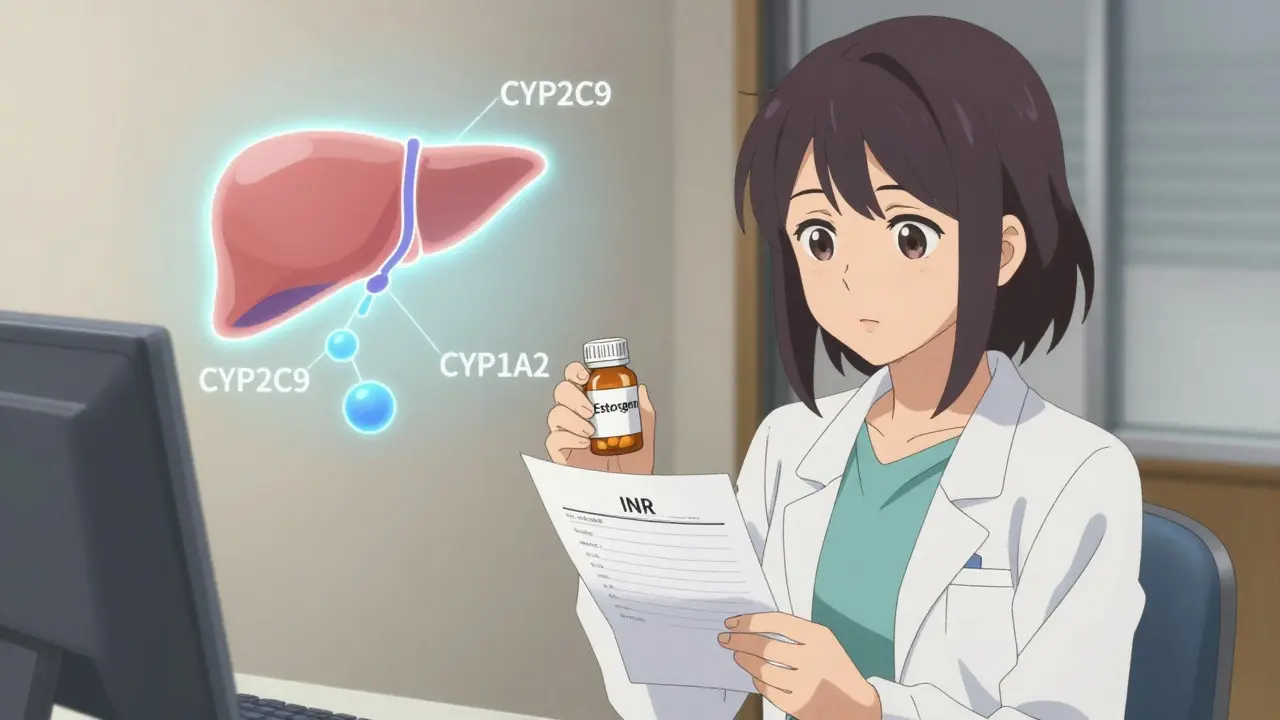
Warfarin doesn't work the same way in everyone. It's broken down in the liver by enzymes called CYP450s, mainly CYP2C9, CYP1A2, and CYP3A4. Estrogen compounds-like estradiol in HRT or ethinyl estradiol in birth control pills-can mess with these enzymes. But here's the twist: they don't all do the same thing.
Natural estrogen (estradiol) tends to speed up warfarin metabolism. That means your body clears it faster, which can drop your INR. On the flip side, synthetic estrogen (ethinyl estradiol) often slows down metabolism, making warfarin stick around longer and raising your INR. This isn't just theory-it's been seen in real patients. One 2009 case study tracked a woman whose INR jumped from 2.4 to 4.3 within five days of starting a birth control pill. Her warfarin dose had to be cut by 30% to get back in range.
That’s why you can’t treat all estrogen the same. A woman on HRT might need a different approach than a teenager on birth control. And it gets more complicated because warfarin itself is a mix of two forms: S-warfarin (stronger, broken down by CYP2C9) and R-warfarin (weaker, handled by CYP1A2 and CYP3A4). Estrogen can hit one pathway harder than the other, leading to unpredictable changes in blood thinning.
How Big Are the Changes? Real Numbers
Not every interaction leads to a crisis. Most estrogen-warfarin shifts cause INR changes between 0.5 and 1.5 units. Sounds small? Think again. For someone with a target INR of 2.5, a jump to 4.0 means their risk of bleeding more than doubles. A drop to 1.0? That’s like turning off your anticoagulation entirely.
Data from the INR Registry, which tracked over 15,000 patients, found that women aged 18 to 45 taking estrogen-containing contraceptives had nearly double the risk of INR levels above 4.0. That’s not rare. In fact, one 2021 survey of 247 pharmacists showed that 68% had managed at least one significant interaction in the past year. Nearly half of those cases required warfarin dose adjustments of 15% to 25%.
Compare that to other common interactions. Antibiotics like ciprofloxacin or metronidazole can spike INR by 2.5 to 3 times. But estrogen? It’s quieter, sneakier. It doesn’t always scream danger-it just nudges the needle. That’s why it’s easy to miss… until someone bleeds.
Genetics Play a Bigger Role Than You Think
Why do some people handle this interaction fine, while others crash into danger? Genetics. About 30% of people carry a variant in the CYP2C9 gene-either *2 or *3-that makes them break down warfarin much slower. Combine that with estrogen that inhibits the same enzyme, and you’ve got a perfect storm.
Then there’s VKORC1. If you have the -1639G>A variant, your body needs 30% to 50% less warfarin to reach the right INR. Add estrogen on top? You might need less than half the dose you’d expect. These aren’t rare mutations. They’re common enough that testing for them is now part of standard care in many U.S. clinics.
The International Warfarin Pharmacogenetics Consortium found that using genetic data to guide warfarin dosing improves accuracy by 30% to 35%. That’s huge. If you’ve been on warfarin for a while and your dose keeps changing, ask if genetic testing was ever done. It might explain why things have been so unstable.
What to Do When Starting or Stopping Estrogen
Don’t wait for symptoms. If you’re on warfarin and you start estrogen-whether it’s a pill, patch, or IUD-get your INR checked within 3 to 5 days. Then check again at 7 to 14 days. The same goes if you stop estrogen. Changes don’t always show up right away. It can take days for the enzyme shifts to fully kick in.
Here’s a simple rule of thumb:
- If INR rises more than 0.5 units: reduce warfarin by 10% to 25%
- If INR drops more than 0.5 units: increase warfarin by 10% to 20%
These aren’t hard numbers-your doctor will adjust based on your history, age, weight, and other meds. But the pattern is clear: monitor early, adjust fast.
And don’t forget: estrogen isn’t just in pills. Some vaginal creams, patches, and even certain herbal supplements (like black cohosh) have estrogen-like effects. If you’re on warfarin, assume anything hormonal needs checking.

Why This Matters More Than You Realize
Over 2.5 million Americans are on warfarin right now. Around 9.7 million U.S. women aged 15 to 49 use hormonal birth control. That’s a lot of overlap. And while newer blood thinners like apixaban or rivaroxaban have fewer interactions, they’re not for everyone. People with mechanical heart valves, severe kidney disease, or antiphospholipid syndrome still need warfarin. For them, estrogen interactions aren’t just a footnote-they’re a daily risk.
The American Heart Association says drug interactions are the second most common cause of anticoagulation-related bleeding, right after missed doses. And estrogen? It’s one of the most common hormonal triggers. Yet, most guidelines don’t scream about it. They just whisper: “Monitor.”
That’s why awareness matters. If you’re a woman on warfarin and you’re considering birth control, HRT, or even menopause treatment, talk to your anticoagulation clinic before you start. Don’t assume your OB-GYN or primary care doctor knows the full picture. Many don’t. A 2021 survey found that 57% of pharmacists found it “moderately to extremely difficult” to tell whether an INR change was from estrogen, diet, illness, or something else.
What’s Changing Now?
Things are getting better. In January 2023, the FDA updated warfarin’s label to include clearer guidance on genetic testing. More clinics now use electronic INR monitoring systems that flag potential interactions before they become problems. One study showed these systems cut estrogen-related adverse events by 32%.
And there’s more coming. The NIH-funded WARFARIN-PREDICT study is building a tool that uses your genetics, age, weight, meds, and estrogen type to predict how your INR will react. It’s still in testing, but early results look promising.
Still, warfarin isn’t going away. Experts predict over 1.8 million Americans will still need it in 2030. That means learning how estrogen affects it isn’t optional-it’s essential.
Can I take birth control pills while on warfarin?
Yes, but you need close monitoring. Birth control pills containing ethinyl estradiol can raise your INR, increasing bleeding risk. Get your INR checked within 3 to 5 days of starting the pill, then again at 7 to 14 days. Your warfarin dose may need to be lowered by 10% to 25%. Don’t switch brands or types without checking your INR again.
Does HRT affect warfarin differently than birth control?
It can. HRT often uses natural estradiol, which may speed up warfarin breakdown and lower INR. Birth control usually contains synthetic ethinyl estradiol, which tends to slow breakdown and raise INR. But it’s not that simple-dose, route (pill vs. patch), and your genetics matter. Always monitor INR when starting or stopping any estrogen therapy, regardless of type.
Why did my INR drop when I started estrogen?
If you’re using natural estradiol (common in HRT), it can induce liver enzymes that break down warfarin faster. This lowers your INR, which means your blood clots more easily. It’s less common than INR spikes, but it happens-especially if you’re on a higher dose of estradiol. Your doctor may need to increase your warfarin dose by 10% to 20%.
Should I get genetic testing if I’m on warfarin and estrogen?
Yes, especially if your INR is hard to control. Variants in CYP2C9 and VKORC1 genes can make you extra sensitive to estrogen interactions. Genetic testing helps predict your ideal warfarin dose and makes managing changes more accurate. Many clinics now offer it as part of routine anticoagulation care.
Are there safer alternatives to warfarin if I need estrogen?
Direct oral anticoagulants (DOACs) like apixaban or rivaroxaban have far fewer interactions with estrogen. But they’re not right for everyone. If you have a mechanical heart valve, severe kidney disease, or antiphospholipid syndrome, warfarin is still the only safe choice. Talk to your hematologist before switching. For others, DOACs may be a better fit.





Comments
Sarah B
Estrogen and warfarin? Yeah I've seen this go south in ER. No one talks about it until someone's bleeding out. Get your INR checked before you even think about starting that pill. Simple as that. No drama.
Tola Adedipe
This is exactly why we need better communication between pharmacists and OB-GYNs. I had a patient last month whose INR went from 2.8 to 4.9 after switching birth control brands. She didn't even know the new pill had ethinyl estradiol. Her doctor didn't either. We got lucky she didn't have a stroke.
Eric Knobelspiesse
so like... i was reading this and i started thinking about how we treat hormones like they're these simple levers when really they're like... quantum soup in a human body? like cyp450s arent just on/off switches they're like mood rings for your liver?? and dont even get me started on how 'natural' estrogen is still just a molecule that binds to receptors like a key in a lock that got filed down a little. also i typoed 'cyp' as 'cyp' again lmao
Marcus Jackson
The data here is solid. But most docs still treat this like a footnote. If you're on warfarin and estrogen, you're not just a patient. You're a lab experiment waiting to happen. Get tested. Track your INR. Don't rely on your doctor to remember every possible interaction.
Natasha Bhala
I'm on warfarin and started HRT last year. My INR dropped from 2.6 to 1.9. My pharmacist caught it before my doc even saw the result. She said 'hormones are sneaky' and I believed her. Just keep monitoring. You got this.
Jesse Lord
I'm a nurse and I've seen this happen too many times. A woman comes in for her INR check, says she started a new pill, and we find her INR doubled. She didn't think it mattered. She thought 'it's just birth control'. But it's not. It's chemistry. And chemistry doesn't care if you think it's small.
Catherine Wybourne
I'm from the UK and we don't talk about this enough either. The NHS still treats warfarin like it's 1999. I had to explain to my GP why my INR spiked after switching to a patch. He said 'but it's not a pill'. I said 'it's still estrogen'. He blinked. Twice.
Amit Jain
THIS IS WHY AMERICA IS BROKEN. We let women take estrogen like candy while their blood turns to soup. No one checks. No one cares. Just give her a pill and tell her to 'monitor'. Meanwhile, her liver is doing backflips. This isn't healthcare. This is Russian roulette with a prescription pad.
Ritu Singh
The scientific evidence presented herein is both robust and compelling. It is imperative that clinical protocols be revised to incorporate mandatory INR monitoring within seventy-two hours of initiating any estrogenic therapy. Furthermore, genetic screening for CYP2C9 and VKORC1 polymorphisms should be considered a standard of care, not an exception.
Mark Harris
You're not alone. I started HRT and my INR dropped. I panicked. Called my anticoag clinic. They adjusted my dose in 10 minutes. Now I check every time I get a new prescription. Small steps. Big safety net.