When bipolar disorder doesn’t respond to mood stabilizers alone, doctors sometimes add an antipsychotic like loxapine. It’s not a first-line choice, but for people stuck in severe mania or mixed episodes-where mood swings crash between highs and lows-loxapine can be the missing piece. Unlike some antipsychotics that make you feel foggy or sluggish, loxapine works fast, often cutting down agitation and aggression within hours. But it doesn’t replace lithium, valproate, or lamotrigine. It works with them. And that combination matters.
What Loxapine Actually Does in the Brain
Loxapine is an older antipsychotic, first approved in the 1970s. It blocks dopamine D2 receptors, which helps calm the overactive brain signals that drive psychosis and severe mania. But it also affects serotonin receptors, which gives it a broader effect than older drugs like haloperidol. This dual action makes it useful not just for hallucinations or delusions, but for the intense irritability, racing thoughts, and impulsivity that come with bipolar mania.
What sets loxapine apart is how quickly it works. Inhaled loxapine (Adasuve), approved in 2018, can reduce agitation in as little as 10 minutes. That’s why it’s often used in emergency rooms or inpatient units. But for long-term management, oral loxapine is more common. It doesn’t fix the underlying mood cycling-but it quiets the storms so mood stabilizers can do their job.
Why Mood Stabilizers Alone Aren’t Always Enough
Mood stabilizers like lithium, valproate, and carbamazepine are the backbone of bipolar treatment. They help prevent both manic and depressive episodes over time. But studies show that up to 40% of people don’t respond well to them alone. Some have breakthrough mania. Others get stuck in mixed states-feeling energized and depressed at the same time-where mood stabilizers alone don’t cut it.
That’s where loxapine comes in. A 2022 analysis of clinical trials found that adding loxapine to a mood stabilizer improved symptom scores by 30-45% more than the stabilizer alone in patients with acute mania. The effect was strongest in those with high levels of aggression or psychosis. It didn’t work for everyone, but for those who needed it, the difference was clear.
How the Combination Works in Practice
Doctors don’t just toss loxapine into a regimen. They follow a careful process:
- Start with a mood stabilizer first-usually lithium or valproate-and give it 4-6 weeks to take effect.
- If symptoms like irritability, loud talking, risky behavior, or sleeplessness persist, add loxapine at a low dose: 5-10 mg per day.
- Monitor for side effects: drowsiness, dry mouth, dizziness, or muscle stiffness.
- After 2-4 weeks, reassess. If agitation is gone but mood is still unstable, adjust the mood stabilizer dose instead of increasing loxapine.
- Goal: Use the lowest effective loxapine dose for the shortest time possible.
Some patients stay on it for months. Others only need it during a crisis. It’s not meant to be a lifelong pill unless other options have failed.

Side Effects and Risks to Watch For
Loxapine isn’t risk-free. The biggest concern is extrapyramidal symptoms-muscle stiffness, tremors, restlessness. These are more common in younger adults and can be mistaken for worsening mania. If they show up, doctors often add a low dose of benztropine or diphenhydramine to counter them.
Another issue: sedation. Loxapine can make you sleepy, especially at first. That’s why many take it at night. But if you’re already on a sedating mood stabilizer like valproate, the combination can be too much. Blood pressure drops and slowed breathing are rare but possible, especially in older adults or those with lung conditions.
There’s also a small risk of tardive dyskinesia-a movement disorder that can become permanent. That’s why doctors avoid using loxapine long-term unless absolutely necessary. Regular check-ins every 3-6 months are standard to catch early signs.
Who Benefits Most From This Combo?
This combination isn’t for everyone. It’s best suited for:
- People with bipolar I disorder in acute mania or mixed episodes
- Those who’ve had poor response to mood stabilizers alone
- Patients with aggression, impulsivity, or psychotic features during episodes
- Those who need rapid symptom control in a hospital or crisis setting
It’s usually avoided in:
- People with Parkinson’s disease or severe movement disorders
- Those with a history of seizures
- Patients with heart rhythm problems (like prolonged QT interval)
- Older adults with dementia-related psychosis (it’s not approved for this)
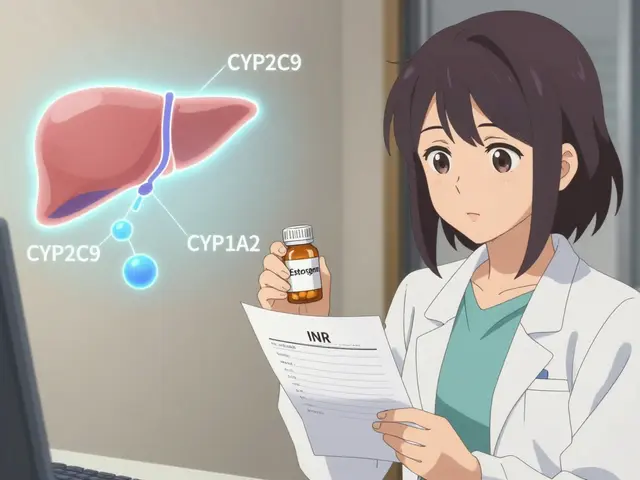
If you’re on lithium, your doctor will check your kidney and thyroid function regularly. If you’re on valproate, liver enzymes and blood counts need monitoring. Loxapine doesn’t interact badly with these, but the added stress on your body means more tests, not fewer.

Alternatives to Loxapine in Combination Therapy
Loxapine isn’t the only antipsychotic used with mood stabilizers. Others include:
| Medication | Speed of Action | Common Side Effects | Long-Term Use Risk |
|---|---|---|---|
| Loxapine | Fast (hours to days) | Drowsiness, muscle stiffness, dry mouth | Moderate (tardive dyskinesia) |
| Olanzapine | Fast | Weight gain, increased appetite, high blood sugar | High (metabolic syndrome) |
| Quetiapine | Medium (days to weeks) | Drowsiness, dizziness, weight gain | High (metabolic effects) |
| Aripiprazole | Slow to medium | Restlessness, nausea, insomnia | Low (but can cause akathisia) |
| Risperidone | Fast | Weight gain, high prolactin, movement issues | Moderate |
Loxapine is less likely to cause weight gain or diabetes than olanzapine or quetiapine. That’s a big plus for people who’ve struggled with metabolic side effects. But it’s more likely to cause muscle stiffness than aripiprazole. The choice depends on your history, your body’s response, and what you can tolerate.
Real-Life Example: Sarah’s Story
Sarah, 34, had bipolar I for 12 years. She’d been on lithium for years, but every 6-8 months, she’d crash into mania-spending money recklessly, staying up for days, yelling at coworkers. Her lithium levels were perfect, but the episodes kept coming.
Her psychiatrist added loxapine 10 mg at night. Within 5 days, she started sleeping. Within two weeks, she stopped making impulsive decisions. She didn’t feel numb-just calmer. She stayed on the combo for 8 months, then slowly tapered off loxapine. She’s been stable for 14 months now, still on lithium alone.
Her story isn’t unique. Many people find that loxapine gives them breathing room-enough time for the mood stabilizer to do what it’s meant to do.
What to Do If You’re Considering This Combo
If you’re on a mood stabilizer and still struggling:
- Track your symptoms: Use a mood journal to note energy levels, sleep, irritability, and risky behavior.
- Ask your doctor: “Could adding an antipsychotic help?” Don’t assume it’s a last resort-it’s a tool.
- Discuss side effects upfront: Know what to watch for and when to call your doctor.
- Don’t stop or change doses on your own: Loxapine withdrawal can trigger rebound mania.
There’s no shame in needing more than one medication. Bipolar disorder is complex. Sometimes, two drugs working together are better than one alone.
Can loxapine be used for bipolar depression?
No, loxapine is not approved or recommended for bipolar depression. It’s primarily used for mania and mixed episodes. For depressive phases, doctors typically turn to lamotrigine, quetiapine, or lurasidone-all of which have evidence for treating low mood in bipolar disorder. Using loxapine during depression may worsen fatigue or apathy.
How long should I stay on loxapine?
Most people take loxapine for a few weeks to a few months during an acute episode. Once mood stabilizers start working and symptoms stabilize, doctors aim to taper off loxapine slowly. Long-term use is rare and only considered if other treatments have failed. Regular check-ins help determine when it’s safe to stop.
Does loxapine interact with alcohol or other drugs?
Yes. Alcohol can increase drowsiness and lower blood pressure when taken with loxapine, raising the risk of falls or fainting. It also interacts with other sedatives, opioids, and some anti-seizure medications. Always tell your doctor about everything you’re taking-including over-the-counter sleep aids or herbal supplements.
Is loxapine better than newer antipsychotics?
It’s not necessarily better-it’s different. Newer drugs like aripiprazole or lurasidone have fewer metabolic side effects, but loxapine acts faster and is less likely to cause weight gain. For someone who’s already overweight or diabetic, loxapine may be preferred. For someone with muscle stiffness issues, a newer drug might be safer. The best choice depends on your personal health profile.
Can I take loxapine if I’m pregnant?
Loxapine is classified as Category C in pregnancy, meaning animal studies showed harm, but human data is limited. If you’re pregnant or planning to be, talk to your doctor. Uncontrolled bipolar episodes can be riskier than medication in some cases. Alternatives like lithium or lamotrigine are often preferred during pregnancy, but if you’re already stable on loxapine, your doctor may keep you on it with close monitoring.
If you’ve tried mood stabilizers and still feel out of control, you’re not failing. You’re just dealing with a complex illness that sometimes needs more than one tool. Loxapine isn’t a cure, but for many, it’s the bridge back to stability.





Comments
Ramesh Deepan
Been on lithium for 8 years and still had those wild manic bursts. Adding loxapine was a game-changer. Didn’t feel zombie-like like with olanzapine. Just… calmer. Like my brain finally stopped screaming. Took about 5 days to notice the shift. Still on it 6 months in, but my doc says we’ll try tapering soon. If you’re stuck, don’t give up-this combo saved my job and my relationships.
Wayne Rendall
It is important to note that loxapine, while effective for acute mania, does not possess FDA approval for the treatment of bipolar depression. This distinction is clinically significant and should be clearly communicated to patients to avoid therapeutic missteps. Furthermore, extrapyramidal symptoms, though manageable, require proactive monitoring, particularly in younger populations.
Ifeoluwa James Falola
Loxapine works fast. That’s the real win. My cousin was in the ER with aggression, couldn’t even sit still. Inhaled loxapine-10 minutes later, he was calm enough to talk. No sedation, no fog. Just quiet. Hope this helps others know it’s not just for psychosis.
Adam Phillips
So like… if the mind is a storm and mood stabilizers are the clouds slowly clearing… then loxapine is the lightning rod that stops the house from burning down right? Like… we’re not fixing the weather we’re just making sure the structure doesn’t collapse while the sky figures itself out
Julie Lamb
This gave me hope 😭 I’ve been on lamotrigine for years but still feel like I’m drowning in mania sometimes. I’m gonna talk to my psych tomorrow. You’re not alone, and you’re not broken. This combo might be your bridge too 💛
april kakoske
it’s not about being fixed it’s about being held… loxapine doesn’t cure bipolar it just lets you breathe long enough to find yourself again… i’ve been on it for 11 months and now i remember what silence feels like… no more racing thoughts just… quiet…
Pradeep Meena
Why do western doctors always give drugs? In India we use yoga and meditation. This loxapine is just a scam by big pharma. Why not try natural healing? You people are too weak. Our ancestors didn’t need pills.
Rishabh Jaiswal
LOXAPINE ISNT EVEN ON THE LIST OF BEST ANTIPSYCHOTICS FOR BIPOLAR IM SORRY BUT I KNOW MORE THAN YOUR DOCTOR LOL I READ A STUDY ON RESEARCHGATE AND OLANZAPINE IS WAY BETTER FOR WEIGHT GAIN AND ITS LIKE 3X MORE EFFECTIVE
May Zone skelah
Oh my god, I just read this and I’m crying. It’s like someone finally articulated the unspeakable. The feeling of being trapped inside your own mind, screaming but no one hears you. Loxapine didn’t just calm me-it gave me back my soul. I used to think I was broken beyond repair. Now I know I was just waiting for the right key. This isn’t medicine. This is poetry written in pharmacology.
Dale Yu
you think this is helping? everyone on here is just drugging themselves into oblivion. you dont need pills you need to face your trauma. your brain is not broken its just scared. stop letting corporations control your mind. this is what they want you to believe. you’re not sick you’re sold
Kshitij Nim
Hey if you're thinking about this combo-start low, go slow. My doc put me on 5mg at night. First week I was sleepy as hell, but after that, the edge went away. No more yelling at my kid over spilled milk. That’s worth a little drowsiness. And yeah, you can get off it later. It’s a bridge, not a cage.
Scott Horvath
just saw someone say loxapine made them feel numb… and i had to laugh because i felt like i was finally awake for the first time in 10 years. its not about feeling nothing its about not feeling like your brain is on fire. i used to think calm meant dead inside. turns out calm just means you can hear yourself think again
Armando Rodriguez
Thank you for this comprehensive and clinically accurate overview. The distinction between acute symptom control and long-term mood stabilization is crucial, and the structured approach to titration and monitoring reflects best practices in psychiatric care. This is precisely the kind of nuanced discussion that empowers patients and reduces stigma. Well done.