Every year, thousands of people end up in the hospital not because their medication didn’t work, but because something they ate, drank, or took as a supplement made it work too well-or not at all.
It’s not just about mixing pills. It’s about that grapefruit in your breakfast smoothie, the garlic pill you started for heart health, or the St. John’s wort you took for low mood while on antidepressants. These aren’t rare exceptions. They’re common, dangerous, and often invisible.
How Interactions Actually Happen
Drug interactions don’t just happen randomly. They follow predictable patterns, mostly through two biological pathways: pharmacodynamic and pharmacokinetic.
Pharmacodynamic interactions occur when two substances affect the same system in your body, either boosting or canceling each other out. For example, if you’re taking warfarin to thin your blood and you start eating large amounts of spinach or kale, the vitamin K in those greens directly fights warfarin’s effect. One study showed that eating just 150 grams of cooked spinach can reduce warfarin’s effectiveness by 30-40% in less than a day. That’s enough to raise your risk of a stroke or blood clot.
On the flip side, combining hawthorn (a popular herbal supplement for heart health) with digoxin-a heart medication-can dangerously strengthen heart contractions. This isn’t theoretical. It’s been documented in clinical studies and led to emergency hospitalizations.
Pharmacokinetic interactions are sneakier. They change how your body absorbs, breaks down, or removes a drug. The most common culprit? The liver’s CYP3A4 enzyme system. It handles about half of all prescription drugs. Now imagine something like St. John’s wort comes along and tells your liver: “Work faster!” Suddenly, your blood pressure meds, birth control, or antidepressants get broken down too quickly. A 2000 study found that St. John’s wort can slash cyclosporine levels by 50-70% in just two weeks. That’s enough to cause organ rejection in transplant patients.
The Grapefruit Trap
Grapefruit isn’t just a tart breakfast fruit-it’s a silent drug amplifier. Its furanocoumarins permanently block the CYP3A4 enzyme in your gut. That means when you take a statin like simvastatin, your body can’t break it down properly. Blood levels can spike up to 15 times higher than normal.
What happens then? Rhabdomyolysis. That’s when muscle tissue breaks down, floods your bloodstream, and can cause kidney failure. The risk jumps from 0.15 cases per 100,000 people a year to 1.57. That’s a tenfold increase. And it doesn’t matter if you eat half a grapefruit or drink a glass of juice. The effect lasts for days. Even if you take your statin at night and eat grapefruit in the morning, the risk remains.
Other citrus fruits like Seville oranges and pomelos have the same effect. But regular oranges? Safe. Limes? Mostly safe. It’s not about citrus-it’s about specific compounds found only in certain varieties.
Supplements Are Not Always Safe
When you buy a supplement, you’re not buying something regulated like a drug. The FDA doesn’t test them for safety or interactions before they hit shelves. That means a bottle of ginkgo biloba might say “natural” and “safe,” but it’s actually a blood thinner. Combine it with aspirin or warfarin, and you’re increasing your risk of bleeding-sometimes severely.
A 2001 study documented 32 cases of abnormal bleeding linked to garlic supplements when taken with anticoagulants. Another study found ginkgo can prolong bleeding time by 30-50%. That’s not a minor side effect. That’s a medical emergency waiting to happen.
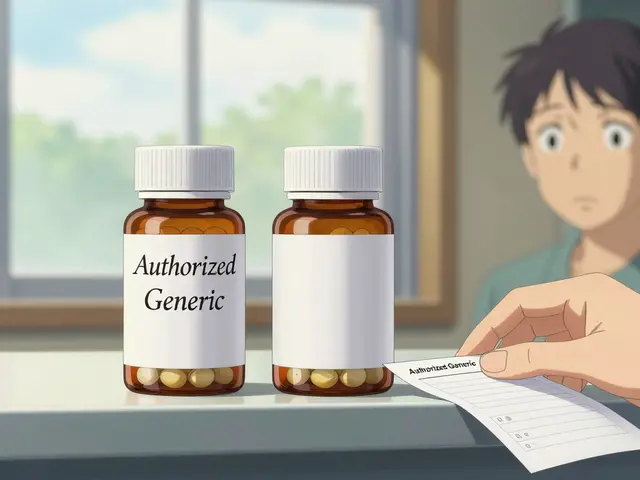
Then there’s red yeast rice. It’s sold as a “natural” cholesterol-lowering supplement. But it contains monacolin K-the same compound as lovastatin, a prescription statin. Taking it alongside your prescribed statin can double or even triple your risk of muscle damage. The Journal of the American College of Cardiology found it increases myopathy risk by 2.3 times.
Coenzyme Q10? Some people take it to boost energy or offset statin side effects. But it might actually reduce how well statins work. And if you’re on an SSRI like sertraline and add St. John’s wort? You could trigger serotonin syndrome-fever, confusion, rapid heartbeat, muscle stiffness. It’s rare, but it kills.
What You Eat Matters More Than You Think
It’s not just grapefruit or leafy greens. Even green tea can interfere with warfarin because of its vitamin K content. Cranberry juice? It’s been linked to over 28 documented cases of dangerous bleeding in people on warfarin, with INR levels shooting past 8.0 (normal is 2.0-3.0). That’s like driving with your brakes stuck.
Dairy products? Calcium in milk and yogurt can bind to antibiotics like tetracycline and ciprofloxacin, making them useless. Take your pill two hours before or after your yogurt.
Alcohol? It doesn’t just make you sleepy. Mixing it with benzodiazepines, painkillers like acetaminophen, or even some antidepressants can overload your liver, increase drowsiness, or cause liver damage. One study found that even moderate drinking while on acetaminophen increased liver injury risk by 300%.
And salt? High sodium intake can make blood pressure meds like diuretics or ACE inhibitors less effective. It’s not just about your heart-it’s about your medication working the way it’s supposed to.
Why People Don’t Tell Their Doctors
Here’s the biggest problem: 70% of people who take supplements never tell their doctor. Why? They think it’s “just a vitamin.” They don’t want to be judged. They assume their doctor already knows.
But doctors don’t ask unless you tell them. And most don’t have time to dig through every pill bottle during a 15-minute visit.
That’s why keeping a written list is non-negotiable. Write down every prescription, over-the-counter pill, herb, vitamin, mineral, and energy drink you take. Update it every time you see a provider-even if you think it’s “not important.”
Pharmacists are your secret weapon. They see your full medication history. Ask them to check for interactions every time you pick up a new prescription. A 2022 study showed pharmacist-led reviews cut adverse events by 22%.
What You Can Do Right Now
- Make a list. Include everything: prescriptions, OTC meds, vitamins, herbs, teas, and even CBD or melatonin.
- Bring it to every appointment. Don’t rely on memory. Show the list to your doctor and pharmacist.
- Ask two questions: “Could this interact with anything I’m already taking?” and “Is there anything I should avoid eating or drinking?”
- Use free tools. The FDA’s MedlinePlus interaction checker lets you search over 3,500 drugs and supplements. It’s free, no sign-up needed.
- Don’t stop meds without talking to your provider. If you’re worried about an interaction, don’t quit cold turkey. You might trigger withdrawal or make your condition worse.
- Be consistent. If you take warfarin, keep your vitamin K intake steady. Don’t go from salads every day to none for a week. Fluctuations are riskier than a steady amount.
What’s Changing in 2025
There’s new momentum. The FDA now requires drug manufacturers to test new medications for interactions with common supplements like St. John’s wort, ginkgo, and echinacea. The Sentinel Initiative is using real-world data from 190 million Americans to track supplement interactions in real time.
AI tools are getting better, too. IBM Watson’s pilot system predicted drug-supplement interactions with 87% accuracy by scanning millions of medical notes. That’s not science fiction-it’s already being tested in hospitals.
But until labels on supplements are required to warn about interactions-like prescription drugs do-you’re still on your own. Only 29% of supplement bottles currently have any interaction warning. That’s not safety. That’s luck.
Bottom Line
Medication safety isn’t just about taking your pills on time. It’s about understanding what else is in your body-and how it talks to your drugs.
You don’t need to avoid all supplements. You don’t need to give up grapefruit forever. But you do need to know the risks. And you need to speak up. The safest thing you can do isn’t a new pill or a fancy diet. It’s a conversation. With your doctor. With your pharmacist. With yourself.
Because when your meds and your meals don’t get along, the consequences aren’t theoretical. They’re real. And they’re preventable.
Can I still eat grapefruit if I’m on medication?
It depends on your medication. Grapefruit can dangerously increase levels of statins (like simvastatin), some blood pressure drugs, and certain immunosuppressants. If you’re unsure, check with your pharmacist or use the MedlinePlus interaction checker. For many drugs, even small amounts can cause problems, so it’s safest to avoid it entirely unless you get a clear green light.
Are natural supplements always safe?
No. “Natural” doesn’t mean safe. Supplements like St. John’s wort, ginkgo, garlic, and red yeast rice have strong, documented effects on medications. Many cause serious interactions because they act like drugs-even though they’re sold as “dietary aids.” The FDA doesn’t test them for safety before sale, so you’re the first line of defense.
Why don’t supplement labels warn about interactions?
Because the Dietary Supplement Health and Education Act of 1994 doesn’t require it. Unlike prescription drugs, supplements aren’t required to prove safety or interaction risks before being sold. Only 29% of supplement labels currently include any interaction warning. That’s changing slowly, but for now, assume every supplement could interact-and check before you take it.
Can I take vitamins with my prescriptions?
Some are fine, others aren’t. Vitamin D and calcium are usually safe with most meds. But vitamin K can interfere with warfarin. Iron can block antibiotics like tetracycline. B vitamins might affect levodopa for Parkinson’s. Always check your specific meds. A simple phone call to your pharmacist takes 2 minutes and could prevent a hospital visit.
What should I do if I think I had a drug interaction?
Stop taking the supplement or food that might be causing it, and contact your doctor or pharmacist immediately. If you experience symptoms like unexplained bruising, bleeding, chest pain, confusion, rapid heartbeat, muscle weakness, or severe drowsiness, go to the ER. Don’t wait. Many interactions can escalate quickly.
Is there a tool I can use to check interactions myself?
Yes. MedlinePlus, run by the National Library of Medicine, offers a free, reliable drug interaction checker that covers over 3,500 medications and supplements. You can search by name without creating an account. It’s the most trusted free tool available. Don’t rely on apps from supplement companies-they’re not always accurate.
How often should I review my medications and supplements?
Every time you see a new provider, start a new medication, or add a supplement-even if it’s “just a multivitamin.” Your body changes. Your meds change. Your habits change. A review every 3-6 months is ideal if you’re on multiple drugs. Keep your list updated in your phone and wallet.






Comments
kora ortiz
Just started taking warfarin and read this-holy crap. I was drinking grapefruit juice every morning. Stopped it today. My pharmacist also told me to keep spinach consistent, not avoid it completely. Small changes, big safety wins.
Jeremy Hernandez
Of course the FDA doesn’t regulate supplements. They’re in bed with Big Herbal. You think they want you to know that your ‘natural’ red yeast rice is basically a stolen statin? Wake up. The system’s rigged. They profit off your ignorance.
Tarryne Rolle
It’s not about interactions. It’s about control. We’ve been taught to fear our own bodies, to outsource health to pills and experts. But what if the real problem is that we’ve forgotten how to listen-to food, to silence, to the rhythm of our own biology?
Kyle Swatt
Man I used to think St. John’s wort was my little mood hack. Then I got put on a new antibiotic and ended up in the ER with a heart that felt like it was trying to punch its way out of my chest. Serotonin syndrome ain’t a vibe. It’s a full-body betrayal. I’m not touching herbal crap unless my pharmacist signs off on it. And even then… I’m nervous.
Deb McLachlin
This is an exceptionally well-researched and clinically relevant piece. The inclusion of specific studies, dosage thresholds, and actionable recommendations elevates it beyond typical health content. I particularly appreciate the emphasis on pharmacist involvement and the MedlinePlus resource. Healthcare systems should integrate such educational frameworks into routine prescribing workflows.
saurabh lamba
so like... if i take turmeric and blood thinner... is it like... bad? or just kinda? idk man i just want to feel good
Kiran Mandavkar
How is it possible that people still believe in ‘natural’ as a synonym for safe? This isn’t the 1800s. We have molecular biology. We have pharmacokinetics. And yet, here we are-people popping ginkgo like candy while on anticoagulants, convinced their ‘holistic lifestyle’ makes them immune to science. It’s not wisdom. It’s arrogance wrapped in hemp.
Eric Healy
grapefruit is fine if u dont take statins but everyone panics over nothing. i eat it every day and my bp is perfect. stop scaremongering
Shannon Hale
Oh my GOD. I just realized I’ve been taking garlic pills with my blood thinner for TWO YEARS. I’m lucky I’m not dead. I’m calling my doctor right now. This post just saved my life. I’m sharing this with EVERYONE. Like, right now. Like, I’m posting it on my mom’s Facebook.
Holli Yancey
I think the most important part is just talking about it. I used to feel dumb asking my doctor about my vitamins. Like, ‘Is this weird?’ But once I started listing everything-even the chamomile tea-I realized how many people are silently scared to speak up. It’s not about being perfect. It’s about being honest.
Gordon Mcdonough
And yet... the government still lets Big Pharma control the narrative. They don’t want you to know how easy it is to kill yourself with a grapefruit and a statin. They want you dependent. They want you buying pills. They want you scared of your own kitchen. This isn’t medicine. It’s corporate control dressed in white coats.
Bill Machi
It's worth noting that the FDA's Sentinel Initiative, while promising, is still in its early stages. Real-time data aggregation from 190 million Americans is an unprecedented undertaking, but the infrastructure for timely intervention remains fragmented. Until standardized electronic health record integration and mandatory supplement labeling are federally enforced, patient responsibility remains the primary-and often only-line of defense. This is not a flaw in individual behavior; it is a systemic failure.