Living with celiac disease isn’t just about avoiding bread or pasta. It’s about relearning how to eat, how to survive, and how to heal your body after years of damage from something invisible-gluten. For 1 in 100 people worldwide, even a tiny crumb can trigger an autoimmune attack that tears apart the lining of the small intestine. And if you’re not careful, that damage leads to serious problems: fatigue, bone loss, anemia, and even higher risk of certain cancers.
What Happens When You Eat Gluten With Celiac Disease
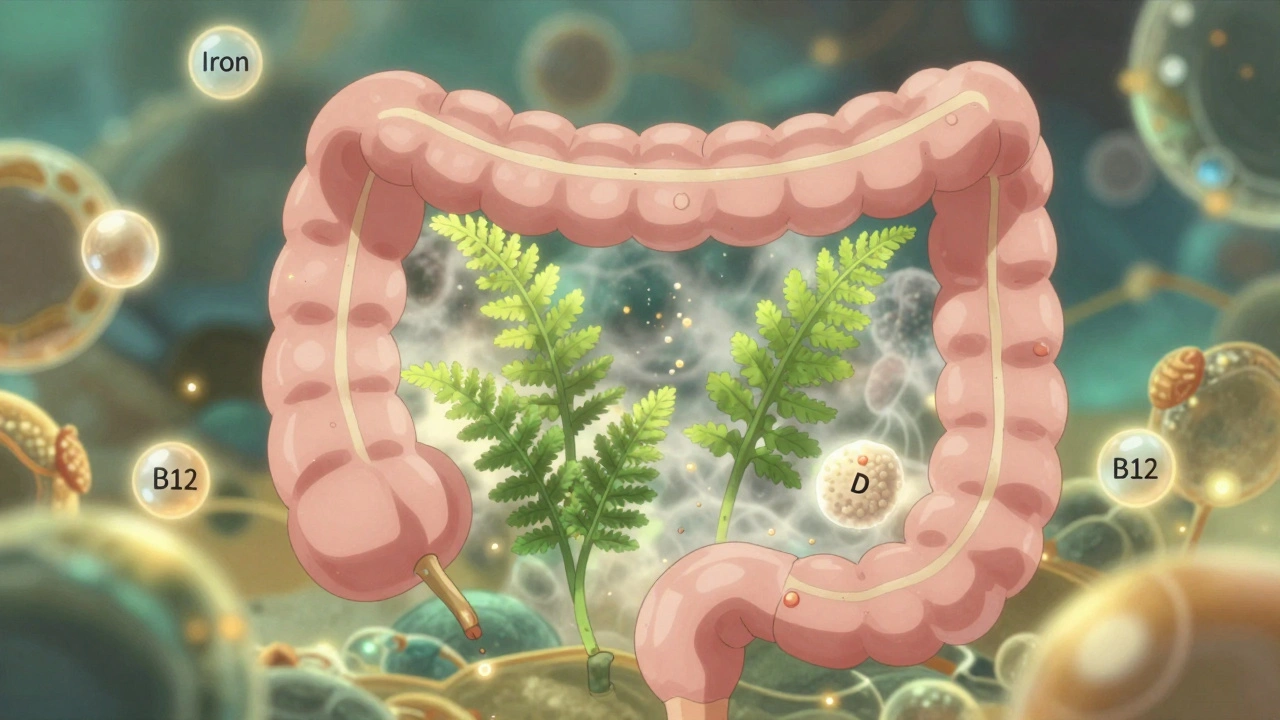
Your immune system doesn’t just dislike gluten-it sees it as an invader. In people with celiac disease, gluten triggers an attack on the villi, the finger-like projections in your small intestine that absorb nutrients. Over time, these villi flatten out. That’s not just inconvenient-it’s dangerous. Without them, your body can’t absorb iron, calcium, vitamin D, B12, or folate properly. You might feel tired, dizzy, or have tingling in your hands and feet. Or you might feel fine, but your bones are quietly crumbling. The only treatment? Complete, lifelong gluten avoidance. No exceptions. No "just a little." Studies show that even 50 milligrams of gluten a day-about the size of a crouton-can stop healing in half of patients. That’s why cross-contamination is just as dangerous as eating gluten on purpose.What Foods Are Actually Safe
You don’t have to eat plain rice and chicken forever. There are plenty of naturally gluten-free foods: rice, quinoa, buckwheat, corn, potatoes, beans, nuts, eggs, meat, fish, dairy, fruits, and vegetables. Certified gluten-free oats are safe for most people, but not all. About 5% of celiac patients still react to them, even when labeled gluten-free. Start slow-no more than 50 grams a day-and watch for symptoms. The real danger? Hidden gluten. Soy sauce? Often contains wheat. Malt vinegar? Made from barley. Some medications? Up to 30% of prescriptions use gluten as a filler. Even communion wafers, play-dough, and lipstick can be sources. That’s why reading labels isn’t optional-it’s survival. And remember: "wheat-free" doesn’t mean gluten-free. Wheat is just one of three gluten grains. Barley and rye are just as dangerous.The Nutrient Deficiencies You Can’t Ignore
At diagnosis, most people with celiac disease are deficient in at least one key nutrient. Here’s what’s most common:- Iron: Affects 12% to 63% of newly diagnosed patients. Causes fatigue, pale skin, and shortness of breath. Oral supplements often don’t work well if the gut is still damaged. Some people need IV iron.
- Vitamin D: 37% to 75% are deficient. Leads to weak bones, muscle pain, and mood issues. Most need 1,000-4,000 IU daily-not the standard 600 IU.
- Calcium: 25% to 40% lack enough. Without it, osteoporosis sets in fast. Aim for 1,000-1,200 mg daily from food and supplements.
- B12 and Folate: Crucial for nerve function and red blood cell production. Deficiency causes numbness, brain fog, and anemia. Sublingual B12 (1,000 mcg) bypasses gut absorption issues.
- Magnesium: Often overlooked. Helps with muscle cramps, sleep, and energy. Many need 400 mg daily.
Testing and Monitoring: What You Need to Track
You can’t guess if you’re healing. You need data.- At diagnosis: tTG-IgA blood test (98% accurate) and total IgA to rule out deficiency.
- At 6 months: Repeat tTG-IgA. Levels should drop by at least 50%. If not, check for hidden gluten.
- At 1 year: Full nutrient panel-iron, ferritin, vitamin D, calcium, B12, folate.
- Every 2-3 years: DXA bone scan to check bone density. Many celiac patients develop osteoporosis without symptoms.
Why Some People Still Feel Sick on a Gluten-Free Diet
If you’re doing everything right but still feel awful, you’re not alone. About 30% of patients have ongoing symptoms despite avoiding gluten. Here’s why:- Hidden gluten: Shared toasters, contaminated oils, restaurant cross-contact. One study found 85% of restaurant-related issues came from shared fryers or grills.
- Slow healing: The gut takes time. Adults often need 1-2 years to fully recover. Kids heal faster.
- Other conditions: SIBO (small intestinal bacterial overgrowth), lactose intolerance, or IBS often coexist. These need separate treatment.
- Non-responsive celiac disease: In 15-30% of cases, the gut doesn’t heal even with perfect diet adherence. This requires advanced testing-like capsule endoscopy-and sometimes immunosuppressants.

Practical Tips for Daily Life
- Buy a dedicated toaster. Even crumbs from regular bread can trigger reactions. - Use gluten-free restaurant cards. The Celiac Disease Foundation offers them in 30+ languages. Show them to servers-it cuts confusion. - Check medications. Use the University of Chicago’s Gluten-Free Drug Database. Many pills contain wheat starch. - Don’t trust labels blindly. Look for "certified gluten-free" (under 20 ppm). Just saying "gluten-free" isn’t enough. - Get a dietitian. Only 78% of major U.S. hospitals have one on staff, but they’re worth their weight in gold. They’ll help you avoid traps and fix nutrient gaps. - Join a community. Reddit’s r/celiac has over 100,000 members sharing real tips. You’re not alone.The Cost and the Future
Gluten-free bread costs nearly 160% more than regular bread. A box of gluten-free pasta? Often $5-$7. That’s a financial burden. Insurance rarely covers supplements or specialized testing-only 15-20% of functional medicine costs are reimbursed. But things are changing. The global gluten-free market hit $8.37 billion in 2024 and is growing fast. More stores carry certified products. New tech like the Nima Sensor lets you test food for gluten in seconds-it detects levels as low as 20 ppm with 90% accuracy. In the future, enzyme therapies and vaccines might help. But right now, the best tool is still the gluten-free diet-done right.What Success Looks Like
People who stick with it don’t just survive-they thrive. Symptoms disappear within days to weeks for 95% of patients. Energy returns. Digestion normalizes. Bone density improves. Anemia clears up. One study found that those who followed the diet strictly had near-normal life expectancy. Those who didn’t? Their risk of death was 2.5 times higher. It’s not easy. But it’s possible. And every meal you eat without gluten is a step toward healing.Can I eat oats if I have celiac disease?
Yes-but only if they’re certified gluten-free. Most oats are contaminated with wheat during farming or processing. Even then, 5% of people with celiac disease react to pure oats. Start with small amounts (50g/day) and monitor for symptoms. If you feel bloated or tired after eating them, stop.
Why am I still anemic after going gluten-free?
Your gut may not have healed fully yet. Iron absorption happens in the small intestine, and damage from celiac disease takes months to repair. You might need higher-dose supplements or even IV iron. Check your ferritin levels-low stores mean your body can’t rebuild red blood cells properly.
Do I need to take supplements forever?
Not forever-but probably for at least a year, maybe longer. Once your gut heals and blood levels normalize, you may reduce or stop some supplements. But vitamin D and calcium often remain necessary, especially if you don’t get enough sun or dairy. Always retest before stopping.
Can celiac disease be cured?
No. There’s no cure yet. The only treatment is lifelong gluten avoidance. But with strict adherence, the gut can fully heal, symptoms disappear, and long-term risks drop to near-normal levels. Research into vaccines and enzyme therapies is ongoing, but nothing is approved yet.
How do I know if my gluten-free diet is working?
Track your symptoms and get blood tests. Your tTG-IgA antibody levels should drop by at least half within 6 months. Your iron, vitamin D, and B12 levels should rise. If you still feel tired, bloated, or achy after a year, talk to your doctor-you might have hidden gluten exposure or another condition like SIBO.
Is it safe to eat at restaurants?
It’s risky. Only 28% of U.S. restaurants have verified gluten-free protocols. Cross-contamination is common-shared fryers, grills, and utensils are the biggest problems. Ask specific questions: "Do you use a separate fryer?" "Can I see the gluten-free menu?" Use a restaurant card. When in doubt, choose simple meals like grilled meat and steamed veggies.







Comments
Ella van Rij
so i just ate a crouton and now my intestines are staging a coup. thanks for the reminder that gluten is basically the dark lord of digestive disorders. 🙃
ATUL BHARDWAJ
in india we have rice, millet, lentils. no need for fancy gluten free bread. simple food heals better.
मनोज कुमार
gluten-free diet is just a trendy placebo for hypochondriacs. 90% of people who claim celiac never got tested. stop selling fear.
Jack Dao
you're lucky you even have access to certified gluten-free oats. in my neighborhood, the only "gluten-free" thing is the air after you leave the grocery store. 🙄
dave nevogt
it's fascinating how a molecular structure as simple as gliadin can unravel an entire physiological system. we think of food as fuel, but for some, it's a landmine disguised as a sandwich. the body doesn't lie-it just whispers until you're forced to listen. healing isn't linear, and the silence between symptoms is often the loudest part of the journey.
Zed theMartian
oh please. you're telling me a 50mg crouton is the end of the world? i've eaten gluten from a shared fryer, a lipstick, and my dog's kibble and still ran a marathon. your gut is weak, not cursed. this is fearmongering dressed as medical advice.
Rebecca M.
so let me get this straight… i have to buy a TOASTER? just for me? and pay $8 for pasta? and test my lipstick? i didn’t sign up for this dystopian food cult. my soul is tired.
Arun kumar
my cousin has celiac and eats only dal and rice. no supplements. no fancy tests. just plain food. maybe we overcomplicate things too much?
Alicia Marks
you got this. every gluten-free meal is a victory. healing takes time but you're already ahead just by being aware. 💪
Jay Everett
the nima sensor changed my life. i tested my friend's "gluten-free" pizza at a joint in Portland-turned out it had 120ppm gluten. i threw it out and bought her a beer. she cried. we both cried. it's not just diet-it's dignity. 🤝
Lynn Steiner
why does everyone assume i'm lying when i say i still feel awful? i'm not lazy. i'm not dramatic. i just have a broken gut and a system that refuses to forgive. and now you're all judging me for needing IV iron? thanks, america.
Steve Enck
the data presented here, while statistically robust, fails to account for the epistemological limitations of self-reported dietary adherence. one cannot assume compliance without biomarker validation, nor can one infer causality from observational cohort data without controlling for confounding variables such as socioeconomic status, access to functional medicine, and psychological comorbidities. the narrative is emotionally compelling but methodologically fragile.