Buprenorphine Dose Calculator
What Makes Buprenorphine Different From Other Opioids?
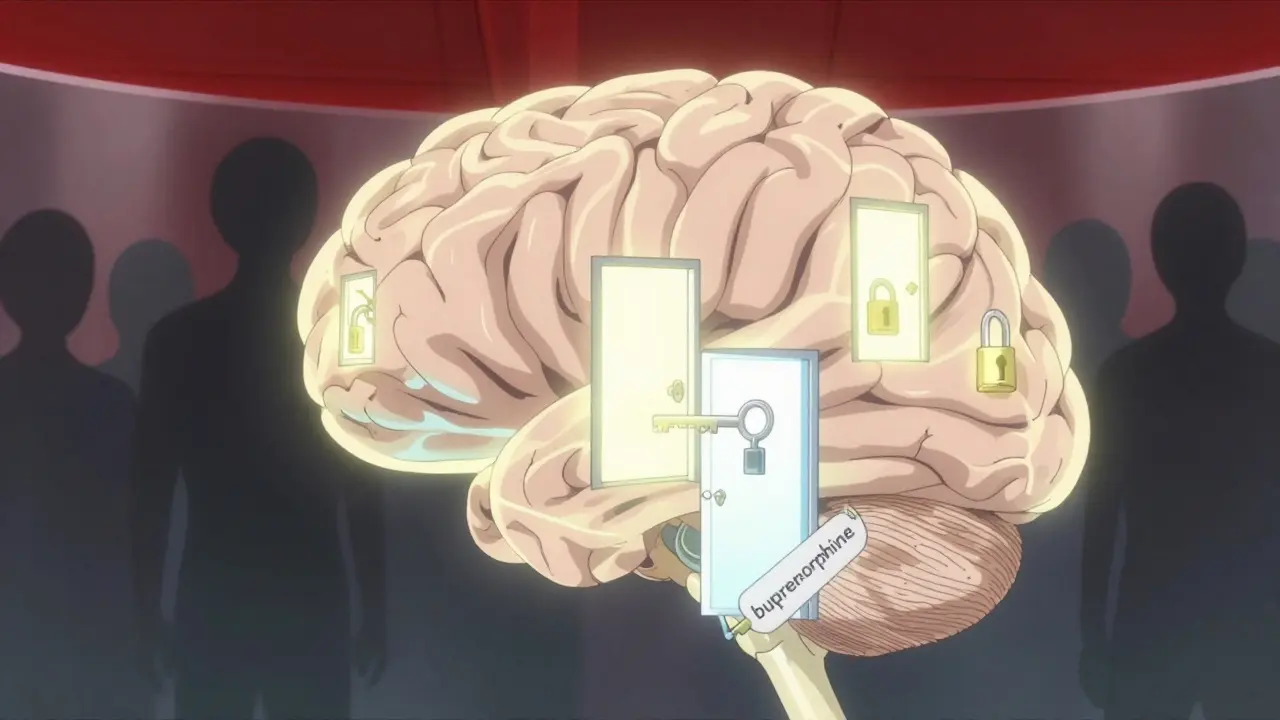
Most people think of opioids as a single group: painkillers that can cause addiction. But buprenorphine isn’t like heroin, oxycodone, or even methadone. It’s a buprenorphine - a partial opioid agonist. That means it activates opioid receptors in the brain, but only partly. It doesn’t turn them all the way on. This small difference is what makes it one of the safest tools we have for treating opioid use disorder.
Imagine you’re turning a dimmer switch. With full agonists like morphine or fentanyl, you can crank it all the way up - and that’s where the danger lies. Too much light, too much opioid effect, and your breathing slows down until it stops. Buprenorphine? It’s like a dimmer with a built-in limit. Once you hit a certain point - around 24 mg per day - turning it further doesn’t make you more high, or more sedated, or more likely to stop breathing. That’s the ceiling effect.
The Ceiling Effect Explained
The ceiling effect isn’t just a buzzword. It’s a measurable, well-documented pharmacological reality. At doses above 24 mg, buprenorphine stops increasing its effects on breathing and heart rate - two of the most dangerous outcomes with opioid overdose. This isn’t theory. It’s been proven in clinical trials going back decades. A 1994 study showed that even doses up to 70 mg didn’t push respiratory depression beyond a certain point. That’s why, even in cases of accidental overdose, buprenorphine alone rarely kills.
But here’s the catch: the ceiling doesn’t apply to everything. For pain relief, the effect can keep rising with higher doses. That’s why some patients with chronic pain on buprenorphine need more than 16 mg - not to get high, but to manage their symptoms. The key is understanding that the ceiling protects you from respiratory failure, not from needing enough medicine to feel stable.
Doctors often say, “It’s not that buprenorphine is weak - it’s that it’s smart.” It binds tightly to opioid receptors, blocking other opioids like heroin or fentanyl from attaching. A 16 mg dose can keep someone from feeling the effects of street opioids for hours. That’s not just treatment - it’s protection.
Why Buprenorphine Is Safer Than Methadone
Methadone has been the gold standard for opioid addiction treatment for over 50 years. But it’s a full agonist. That means it can still cause dangerous respiratory depression, especially when doses are too high or when mixed with alcohol or benzodiazepines. In the U.S., methadone overdose deaths still outnumber those from any other prescription opioid - even when used as directed.
Buprenorphine changes that. Studies show it’s about five times less likely to cause fatal respiratory depression than methadone. In 2022, about half of all medication-assisted treatment prescriptions in the U.S. were for buprenorphine - and that number is still rising. Why? Because patients live longer on it.
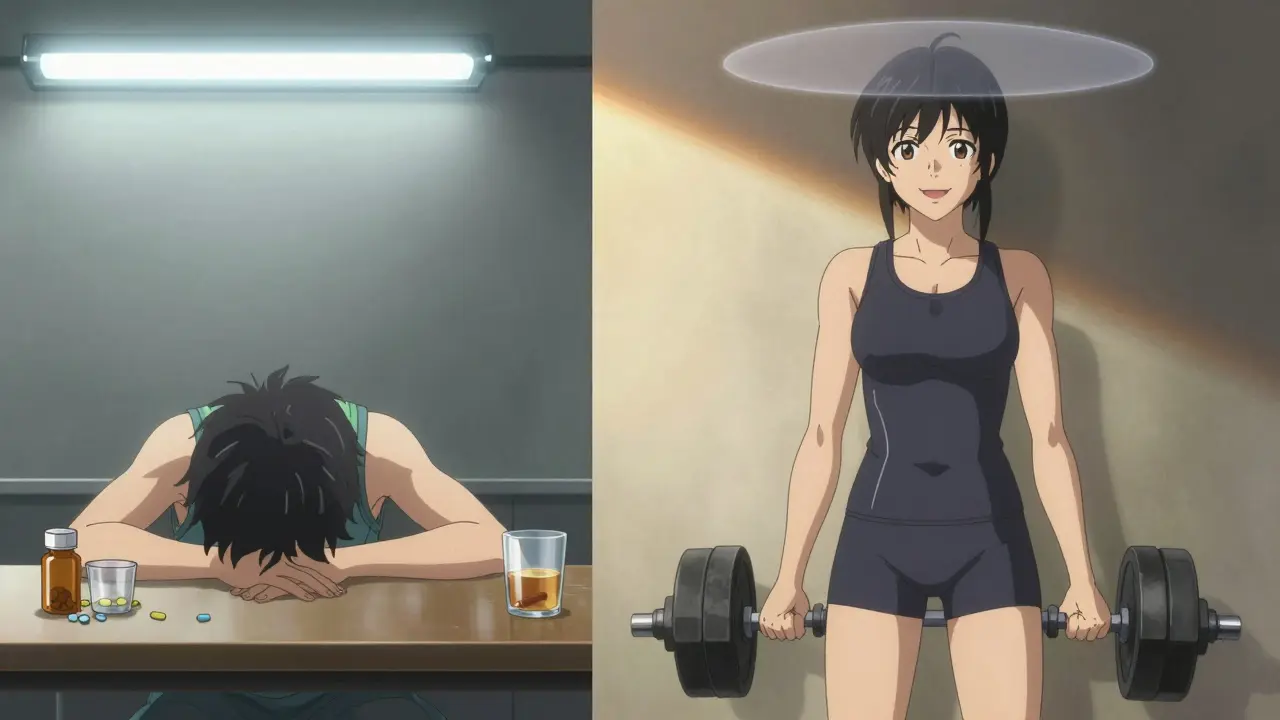
One patient in Bristol told me, “I used to take methadone and couldn’t drive or work without nodding off. Now I take my 12 mg of buprenorphine and go to the gym. I feel normal.” That’s not anecdotal. It’s backed by data. Up to 80% of patients report reduced cravings within an hour of taking buprenorphine, with far less sedation than methadone.
Common Side Effects - And What’s Not a Big Deal
Yes, buprenorphine has side effects. But they’re usually mild - and far less severe than those from full opioids.
- Headache: Affects about 18% of users in early treatment. Usually fades after a few days.
- Constipation: Happens in 12% of patients. Still less than with oxycodone or hydrocodone.
- Nausea: Common at first, especially if taken on an empty stomach. Eating before dosing helps.
- Precipitated withdrawal: This is the most common mistake. If you take buprenorphine too soon after using heroin or fentanyl, it can kick out the other opioids from your receptors and make you sick. That’s why induction has to be timed right - usually 12 to 24 hours after the last full opioid dose.
Some people worry about dependency. Yes, you can become physically dependent on buprenorphine - but that’s not addiction. Addiction is compulsive use despite harm. Dependence is just your body adapting. Thousands of people take buprenorphine for years, even decades, and live full, productive lives. It’s not a crutch - it’s a bridge.
The Real Danger: Mixing With Other Depressants
The biggest risk with buprenorphine isn’t the drug itself. It’s what people mix it with.
A 2022 study in the Journal of Addiction Medicine found 18 fatal overdoses involving buprenorphine between 2019 and 2021. Every single one involved benzodiazepines (like Xanax or Valium), alcohol, or other sedatives. The ceiling effect doesn’t protect you from those combinations. When you stack depressants, your brain loses its ability to keep breathing - even with buprenorphine in your system.
This is why doctors screen for alcohol use, anxiety disorders, and sleep aid use before prescribing. If you’re on buprenorphine, don’t drink. Don’t take sleeping pills unless your prescriber says it’s safe. Don’t assume “it’s just one pill.” That one pill could be the one that stops your breathing.
Dosing: More Isn’t Always Better
There’s a myth that higher doses mean better results. With buprenorphine, that’s not true. Most people stabilize between 8 mg and 16 mg per day. Going above 24 mg doesn’t give you more pain relief, less cravings, or a stronger high - it just increases cost and potential for side effects like dizziness or sweating.
Some patients with severe, long-term opioid use may need 20-24 mg. That’s not because they’re “addicted” - it’s because their receptors are more resistant. A 2023 study from the MCSTAP network found that patients with chronic pain or high tolerance often need higher doses to achieve full receptor blockade. But even then, the ceiling on respiratory depression holds.
Start low. Go slow. Most providers begin with 2-4 mg, then increase in 2-4 mg increments over a few hours on day one. By day three, most people are at their optimal dose. No need to rush.
What About the New Injections?
In 2023, the FDA approved Sublocade - a monthly buprenorphine injection. This is a game-changer for people who struggle with daily pills. No more forgetting doses. No more stigma of picking up a daily script. Clinical trials showed 49% of patients stayed abstinent for 26 weeks - compared to 35% on daily sublingual tablets.
It’s not for everyone. You need to be stable on oral buprenorphine first. And it’s expensive. But for those who need it, it removes a huge barrier to recovery.
Who Shouldn’t Use Buprenorphine?
Buprenorphine is safe for most people - but not all.
- If you’re allergic to buprenorphine or naloxone (in Suboxone), avoid it.
- If you have severe liver disease, your doctor may need to adjust the dose or choose another option.
- If you’re pregnant, buprenorphine is actually preferred over methadone - it causes less neonatal withdrawal in babies.
- If you’re on other opioids, you must wait until you’re in mild withdrawal before starting. Otherwise, you’ll feel sick.
And no - you don’t need to be in therapy to get it. The American Society of Addiction Medicine says treatment shouldn’t be withheld just because counseling isn’t available. Buprenorphine saves lives even on its own.
Final Thoughts: It’s Not Perfect - But It’s Life-Saving
Buprenorphine isn’t magic. It won’t cure addiction. It won’t fix trauma or unemployment or housing instability. But it gives you a chance. It lets you wake up without shaking. It lets you go to work. It lets you be a parent again. It lets you live without the fear of overdose every time you use.
The ceiling effect isn’t just a scientific term. It’s a promise: you can get better without dying. And that’s more than most opioids can say.






Comments
Claire Wiltshire
Buprenorphine’s ceiling effect is one of the most underappreciated advances in addiction medicine. It’s not just safer-it’s profoundly humanizing. People who’ve been told they’re ‘just addicted’ get to reclaim their lives without being treated like walking risks. The data doesn’t lie: this isn’t substitution, it’s restoration.
And yes, the mixing with benzodiazepines is terrifying. We need better public education on that. Not scare tactics-just clear, compassionate facts. This drug saves lives when used correctly, and we owe it to patients to stop stigmatizing the treatment itself.
Darren Gormley
LMAO 🤡 another ‘buprenorphine is magic’ post. Have you seen the withdrawal from this stuff? It’s brutal. And don’t get me started on the black market prices. This isn’t treatment-it’s a new kind of dependency with a fancy label. Also, ‘ceiling effect’? Sounds like a marketing term made by pharma to sell more pills. 🤷♂️
Mike Rose
idk man i think this whole buprenorphine thing is just another way for doctors to make money. people just wanna get high anyway. why not just let em use heroin? at least its cheaper. also i heard it makes you sweat a lot lol
Niamh Trihy
Thank you for writing this with such clarity. The distinction between dependence and addiction is critical-and often misunderstood. I’ve seen too many people dismissed as ‘not sober enough’ because they’re on buprenorphine. Recovery isn’t about being drug-free-it’s about being alive.
The point about precipitated withdrawal is vital too. Many patients get turned away because providers don’t understand timing. This isn’t just pharmacology-it’s dignity.
Yanaton Whittaker
AMERICA IS THE ONLY COUNTRY THAT TREATS OPIOID ADDICTION LIKE A MEDICAL ISSUE. IN MY COUNTRY, WE JUST LOCK THEM UP. BUPRENORPHINE IS JUST A LIBERAL SOCIAL ENGINEERING TOOL. WE NEED MORE POLICE, NOT MORE PILLS. 🇺🇸💪
Sazzy De
i’ve been on 16mg for 3 years. i work full time, i hike on weekends, i’m raising my niece. this isn’t a crutch. it’s the thing that kept me alive. no drama. no hype. just real life. 🌱
Jodi Olson
The pharmacodynamics of partial agonism present a fascinating paradox: maximal receptor occupancy without maximal physiological response. This is not merely therapeutic-it is ontologically significant. We are not treating addiction; we are reconfiguring neurobiological narratives of selfhood. The ceiling effect, then, is not a limit but a liberation.
Carolyn Whitehead
this post made me cry a little. my brother was on methadone for years and kept getting sicker. when he switched to buprenorphine he started cooking again. he took my dog to the park. he remembered my birthday. it’s not perfect but it’s hope. thank you for writing this
Katie and Nathan Milburn
The clinical efficacy of buprenorphine in reducing mortality rates among individuals with opioid use disorder is statistically significant and clinically meaningful. Further, the integration of pharmacological intervention with psychosocial support remains optimal, though not strictly necessary for survival. The data support its broad dissemination.
Beth Beltway
Let’s be honest-this is just enabling. People on buprenorphine are still using drugs. They’re just using a government-approved one. Where’s the accountability? Where’s the ‘just say no’? This isn’t recovery-it’s pharmaceutical welfare. And now we’re giving them injections? Next they’ll be handing out free methadone at Starbucks. This is a national disgrace.
kate jones
Sublocade’s 49% abstinence rate at 26 weeks is remarkable-but it’s not the whole story. We need to look at retention, quality of life, and reduction in criminal justice involvement. Buprenorphine isn’t just about abstinence-it’s about reintegration. For marginalized populations, monthly injections remove stigma, logistical barriers, and daily shame.
Also: the liver disease caveat is crucial. Many providers overlook CYP3A4 metabolism. Always check ALT/AST before prescribing. And yes-pregnancy is a strong indication. Buprenorphine reduces NAS severity compared to methadone. This isn’t theory. It’s practice. And it’s working.