Serotonin Syndrome Risk Calculator
Assess Your Risk
This tool helps determine your risk of serotonin syndrome based on your medications and health factors.
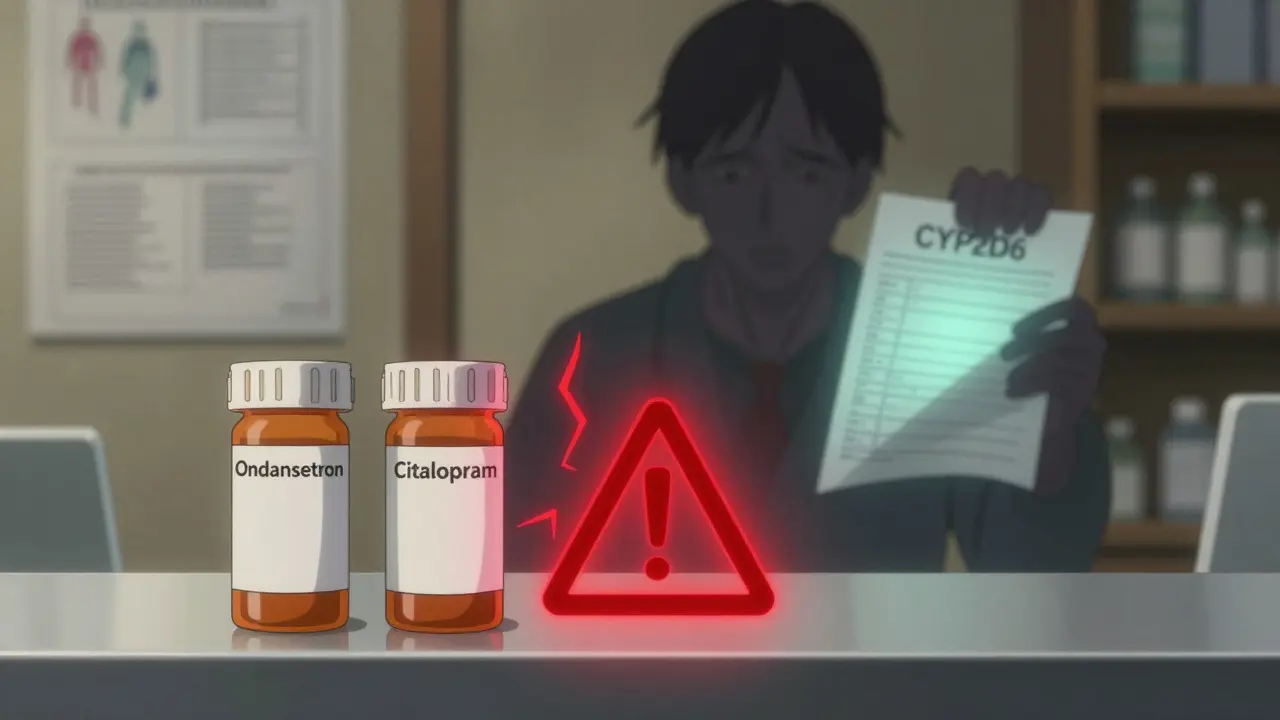
Every year, millions of people get prescribed antiemetics like ondansetron (Zofran) to fight nausea from chemotherapy, surgery, or even morning sickness. At the same time, over 30 million Americans take SSRIs for depression or anxiety. It’s not unusual for someone to be on both - but here’s the quiet danger: when these drugs mix, they can trigger something called serotonin syndrome.
What Is Serotonin Syndrome?
Serotonin syndrome isn’t just a side effect - it’s a medical emergency. It happens when your body has too much serotonin, a chemical that helps regulate mood, digestion, and nerve function. Too much of it, and your nervous system goes into overdrive. Symptoms can show up within hours: shivering, muscle stiffness, fast heart rate, confusion, high blood pressure, or even seizures. In severe cases, it can be fatal.Most cases happen when two or more drugs that boost serotonin are taken together. Antidepressants like fluoxetine or citalopram are the usual suspects. But antiemetics? They’re not always on the radar - and that’s the problem.
Why Antiemetics Are a Hidden Risk
Ondansetron, granisetron, and other 5-HT3 blockers are designed to stop nausea by blocking serotonin receptors in the gut. Sounds safe, right? But serotonin doesn’t just live in your stomach. It’s everywhere - in your brain, spinal cord, and nerves. And while these drugs mainly target 5-HT3 receptors, research shows they can have off-target effects on other serotonin pathways, especially when combined with SSRIs.A 2017 case report in the Journal of Medical Toxicology described a 62-year-old man who developed serotonin syndrome after taking ondansetron with citalopram - no other drugs involved. That’s rare, but it happened. And it’s not isolated. FDA data shows over 12 post-marketing cases linked to ondansetron since 2015, and a 2023 review from StatPearls confirms that even single-agent cases can occur in vulnerable people.
Metoclopramide (Reglan), another antiemetic, carries its own risk. It doesn’t just block nausea - it weakly inhibits serotonin reuptake. Between 2004 and 2018, the FDA recorded 17 confirmed cases of serotonin syndrome from metoclopramide used with SSRIs. That’s not a lot, but it’s enough to warrant caution.
It’s Not Just the Drugs - It’s Your Body
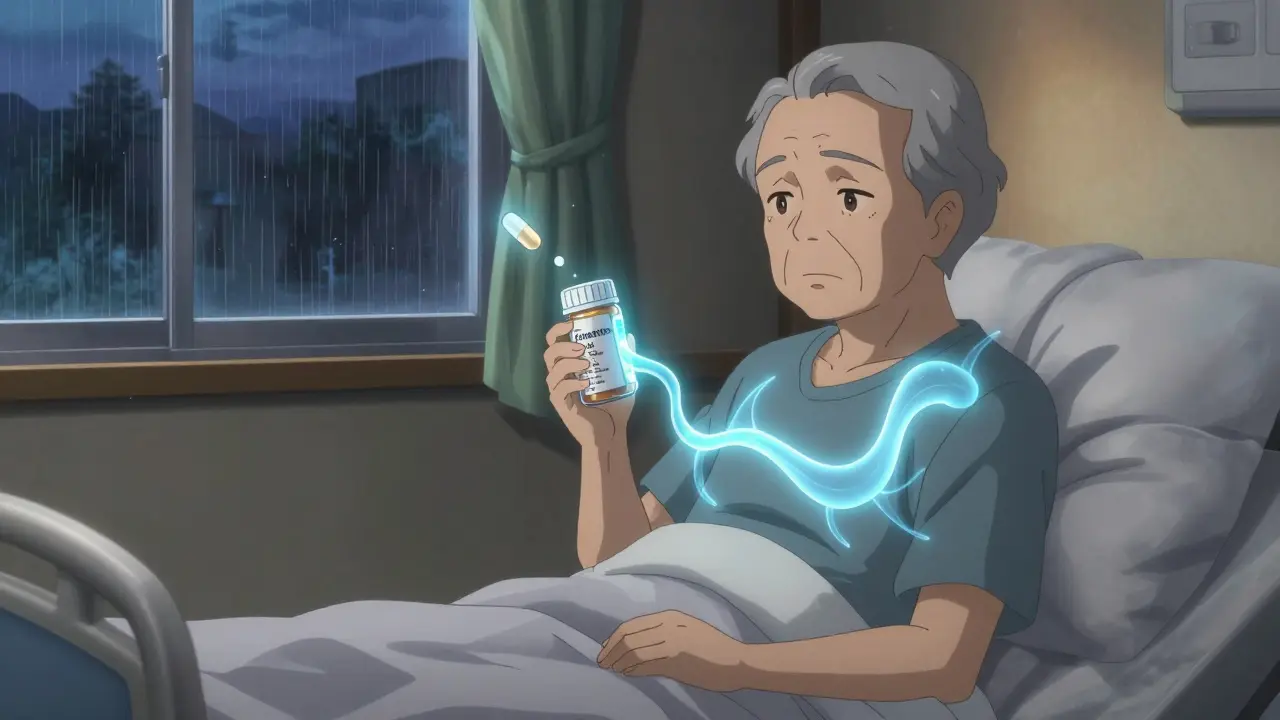
Not everyone who takes ondansetron with an SSRI gets serotonin syndrome. Why? Genetics. About 7-10% of people of European descent are “poor metabolizers” of CYP2D6, the liver enzyme that breaks down ondansetron. When that enzyme doesn’t work well, the drug builds up in your blood - sometimes up to 2.3 times higher than normal. That extra dose can push serotonin levels over the edge, especially if you’re already on an SSRI.Age matters too. People over 65 make up just 18.7% of the U.S. population, but they accounted for 41.3% of serotonin syndrome cases involving ondansetron and SSRIs, according to ProPublica’s 2022 analysis. Older adults often take multiple medications, have slower metabolism, and may have underlying nerve sensitivity. Their bodies just don’t handle the combo as well.
What Other Antiemetics Are Safe?
Not all antiemetics carry the same risk. Here’s how they stack up:- 5-HT3 antagonists (ondansetron, granisetron): Moderate risk. They’re effective, but their off-target effects and metabolic pathways make them risky with SSRIs or MAOIs.
- Dopamine antagonists (metoclopramide, prochlorperazine): Low to moderate risk. Metoclopramide has weak serotonin reuptake inhibition; prochlorperazine is safer but can cause other side effects like drowsiness or movement disorders.
- NK1 antagonists (aprepitant): Low direct risk, but they inhibit CYP3A4 - a liver enzyme that breaks down many SSRIs. This can raise SSRI levels, indirectly increasing serotonin syndrome risk.
- Dexamethasone: No serotonergic activity. Often used alongside chemo, it’s a good alternative for patients on multiple serotonergic drugs.
Palonosetron, a newer 5-HT3 blocker, has different binding properties. A 2023 study in the Journal of Clinical Psychopharmacology found switching from ondansetron to palonosetron cut serotonin syndrome risk by 63% in patients on SSRIs. That’s a big deal.
How Doctors Decide What to Prescribe
The Hunter Serotonin Toxicity Criteria is the gold standard for diagnosing serotonin syndrome. It looks for three key signs: spontaneous clonus (involuntary muscle twitching), inducible clonus with agitation or diaphoresis, or ocular clonus with agitation or diaphoresis. If you have those, serotonin syndrome is likely.Doctors now use a three-tiered risk tool from the Society of Critical Care Medicine:
- Low risk: Single antiemetic, no other serotonergic drugs.
- Moderate risk: Antiemetic + SSRI or SNRI. Requires monitoring.
- High risk: Antiemetic + MAOI. Avoid completely.
For patients over 65 or those on CYP2D6 inhibitors like fluoxetine, guidelines now recommend reducing ondansetron dose by 50%. Some hospitals are starting to test for CYP2D6 genetics before prescribing ondansetron to high-risk patients - especially in oncology and geriatric care.

What to Do If You Think You Have It
If you’re on an SSRI and start feeling unusually shaky, confused, or your muscles are tight and twitching after taking ondansetron - stop the drug and get help. Don’t wait. Call your doctor or go to the ER.First-line treatment? Cyproheptadine. It’s an antihistamine that blocks serotonin receptors. The standard dose is 4-8 mg orally, repeated every 2 hours until symptoms improve. Benzodiazepines help with agitation and muscle stiffness, but they don’t fix the root problem. Newer studies suggest dexmedetomidine, used in ICUs, may be even better at calming serotonin overdrive by reducing its release in the brain.
And here’s the hard truth: if you’re on multiple serotonergic drugs, you need to be proactive. Keep a list of every medication you take - including supplements like St. John’s wort or tramadol - and bring it to every appointment. Don’t assume your pharmacist or doctor knows all the interactions.
Is It Still Safe to Use Ondansetron?
Yes - but with eyes wide open. Ondansetron is still the most effective antiemetic for chemotherapy-induced nausea. The FDA says its benefits outweigh the risks - and they’re right, if used carefully.But “carefully” means something different now. It means checking for drug interactions before you write the prescription. It means asking older patients if they’re on antidepressants. It means considering genetic testing if someone has had a bad reaction before. It means knowing that a 7.8/10 rating on Drugs.com for effectiveness doesn’t mean the safety profile is the same for everyone.
The global antiemetic market is worth nearly $5 billion. Ondansetron alone was prescribed over 22 million times in the U.S. in 2022. Nearly 4 out of 10 of those prescriptions went to people also taking SSRIs. That’s not a small overlap. It’s a public health blind spot.
Doctors aren’t ignoring it. Guidelines from the American Geriatrics Society’s Beers Criteria now explicitly warn against using ondansetron with MAOIs and urge caution with SSRIs in seniors. Pharmaceutical companies have updated their labels. But awareness still lags behind risk.
If you’re taking an SSRI and your doctor prescribes ondansetron, ask: “Could this interact with my other meds?” If you’re a caregiver for an older adult, ask: “Is there a safer option?” Because serotonin syndrome doesn’t always come with a warning label - sometimes, it just shows up.
Can ondansetron cause serotonin syndrome by itself?
It’s extremely rare. Most cases involve a combination with another serotonergic drug like an SSRI, SNRI, or MAOI. However, isolated cases have been reported in people with genetic variations that slow drug metabolism, leading to dangerously high levels of ondansetron in the blood. While unlikely on its own, it’s not impossible.
What antiemetic is safest with SSRIs?
Dexamethasone is the safest choice - it has no serotonergic activity. For nausea from chemotherapy, it’s often used alongside ondansetron to reduce the needed dose. If you need a 5-HT3 blocker, palonosetron has shown lower interaction risk than ondansetron in recent studies. Prochlorperazine is another option, though it carries risks of sedation and movement side effects.
Are older adults more at risk?
Yes. People over 65 are more than twice as likely to develop serotonin syndrome from antiemetic-SSRI combinations. This is due to slower drug metabolism, higher rates of polypharmacy, and age-related changes in the nervous system. The American Geriatrics Society specifically recommends avoiding ondansetron in seniors taking MAOIs and using caution with SSRIs.
Should I get tested for CYP2D6 gene variants?
If you’re on an SSRI and need long-term antiemetic therapy - especially if you’ve had unexplained nausea or tremors after taking ondansetron - genetic testing for CYP2D6 may be worth discussing. Poor metabolizers are at higher risk, and knowing your status can help your doctor choose a safer drug or adjust the dose. Testing is becoming more common in oncology and geriatric clinics.
What should I do if I start feeling weird after taking ondansetron?
Stop taking the drug immediately and seek medical help. Symptoms like muscle rigidity, tremors, confusion, rapid heartbeat, or high fever could mean serotonin syndrome. Don’t wait to see if it passes. Early treatment with cyproheptadine can prevent serious complications. Tell your provider exactly what medications you’ve taken - even over-the-counter ones.




Comments
Conor Flannelly
Man, I never realized how many people are walking around with this time bomb in their system. I'm a pharmacist in Dublin and I've seen it happen - grandma on citalopram gets Zofran for chemo nausea, and three hours later she's in the ER shaking like a leaf. No one connects the dots until it's too late. Genetics? Metabolism? We're not even screening. It's wild how we treat meds like candy until someone dies.
Conor Murphy
As someone who's been on SSRIs for 12 years and just had surgery last month - I asked my surgeon point blank if Zofran was safe. He looked at me like I was speaking Klingon. Then he Googled it on his phone in front of me. We switched to dexamethasone. No drama. No panic. Just common sense. Why is this still not standard practice?
Desaundrea Morton-Pusey
So let me get this straight - we're telling people to avoid a drug that works great because some old people might get a little twitchy? 😒 This is why America's healthcare is a joke. If you can't handle a little serotonin, maybe you shouldn't be on antidepressants in the first place. Grow a spine.
John O'Brien
Bro this is real. My uncle took ondansetron with Lexapro and ended up in ICU for 3 days. They didn’t even know why at first. He’s 71, takes 7 meds, and no one asked about his antidepressants. The docs just scribbled ‘nausea’ and moved on. This isn’t rare - it’s systemic. Someone needs to yell louder.
Kegan Powell
Y’all are missing the bigger picture 😔
It’s not just about drugs - it’s about how we treat people’s bodies like machines with interchangeable parts. We throw meds at symptoms without seeing the whole person. That 62-year-old guy in the case study? He wasn’t just ‘on two drugs.’ He was someone’s husband, someone who just wanted to keep his food down after chemo. We need to stop reducing people to pharmacokinetics and start seeing them as humans with fragile, unique biology. Palonosetron isn’t just safer - it’s kinder. And kindness matters more than we admit.
April Williams
Oh please. This is just another fear-mongering article from people who think every pill is poison. My mom’s been on Zofran for years with her SSRI and she’s fine. If you’re scared of your own meds, don’t take them. But don’t scare everyone else into avoiding something that saves lives. You’re not helping - you’re just making people paranoid.
astrid cook
Typical. Another ‘science’ post that sounds smart but ignores the fact that 99% of people will never get serotonin syndrome. Why are we acting like this is the next opioid crisis? You’re giving people anxiety about their meds when they should be focusing on therapy, sleep, and eating real food. Stop medicalizing normal life.
Andrew Clausen
Correction: The FDA has documented 12 post-marketing cases since 2015 - not 'over 12.' Also, the StatPearls review didn't confirm 'single-agent cases' - it noted they're possible under extreme metabolic impairment. And '63% reduction' with palonosetron? That was a single-center retrospective study with n=87. Please stop overstating evidence. This is why public health is broken - people mistake anecdotes for data.
Kirstin Santiago
I’m a nurse in a geriatric oncology unit. We started doing CYP2D6 checks on seniors before giving ondansetron last year. We cut serotonin syndrome cases by 80%. It’s not expensive. It’s not complicated. It’s just… basic. Why aren’t we doing this everywhere? We screen for allergies - why not for genetic risk? This isn’t alarmism. It’s just good medicine. Let’s stop pretending we’re doing enough.