
Are you one of millions of people battling some type of hair loss? More than half of males experience some degree of male pattern baldness by age 50, but even women and children can experience unwanted hair loss. There are more options than ever before to treat hair loss — such as herbal treatments, scalp massage, lasers, and surgery — but one of the most popular options is the safe and effective pharmaceuticals on the market.
There are two main medications approved by the FDA for treatment of hair loss — and they’re very different. For starters, Rogaine is a topical solution applied to the scalp, while Propecia is an orally administered pill. One medication is better than the other at treating a receding hairline. Men can use either medication, or even both, but women are restricted to just one. Because of these distinctions, it is important to choose the right hair-loss medication for you.
Let’s take a closer look at each one.
Rogaine (minoxidil) was first on the scene. Its ability to fight hair loss was discovered accidentally. The drug, a vasodilator, was originally used exclusively to treat high blood pressure, when some patients began reporting that it re-grew hair as a side effect. It was approved by the FDA in 1988 to treat male pattern baldness. Rogaine, by Pfizer, is primarily effective at stopping hair loss, but in some patients, it can increase protein blocks, which can promote new hair growth. It is said to be effective both on the hairline and vertex of scalp. Rogaine can be used by both men and women, in a 2% or 5% solution.
Propecia (finasteride), made by Merck, is an orally administered medication approved by the FDA in 1997 to treat hair loss. Unlike Rogaine, which is a vasodilator, Propecia acts on hair loss through hormonal means. (Because of this, Propecia should NOT be used by women or children; it could be very dangerous.) Propecia is an anti-androgen, which decreases the conversion of testosterone to dihydrotestosterone (DHT), a chemical responsible for balding. With DHT inhibited, existing hair is better maintained, and the body can put more energy into thinning follicles so that they become thicker. Propecia has high effectiveness with early to moderate hair loss, and works best on the crown of the head, but not as well with a receding hairline.
Neither Rogaine nor Propecia is a quick fix for hair loss. They both need to be taken for long periods. It can take anywhere from 6 to 24 months to see initial results, and patients may need to take their chosen medication indefinitely keep treating the condition.
Knowing all this, which factors should guide your choice between Rogaine and Propecia?
- Your gender: if you are male, you can be prescribed either (or both), but if you are a woman, you can only use Rogaine.
- Your goals: Rogaine is slightly more useful for retaining existing hair, while Propecia is said to be more effective at promoting new hair growth.
- Your area of hair loss: Propecia has good results mainly on the crown, while Rogaine has documented success on the hairline and the crown.
- Medical interactions: Consult your physician to determine which drug is a better fit for your personal health conditions and other medications.
- Side effects: With Propecia, you may experience decreased libido or gynecomastia. Rogaine may trigger allergic effects, chest pain, dizziness, or irregular heartbeat.
- Ease of use: Some people feel that a daily pill is simpler than a twice-daily application to the scalp, but others prefer to pick their medication based on its mode of action.
Whichever method you select, be patient, and remember to keep feeling good about yourself, your hair, and your overall health. As with any drug, please consult your physician before you begin any medication.

Painful conditions of the esophagus and stomach are common in our society. Stress, obesity, poor diet, and smoking can all play a part. Whether you suffer from acid reflux or ulcers, controlling acid is probably part of your game plan for comfort and health. But there are two very similar acid-controlling drugs from the same parent company on the market: Prilosec and Nexium. How does a savvy healthcare consumer evaluate which one is right or them?
The basics:
Prilosec (omeprazole) was introduced in 1989. Nexium (esomeprazole) was released in 2001. These two drugs are very similar chemically — they are both proton pump inhibitors. This means inhibit the secretion of hydrochloric acid. Yet, they are subtly different: Nexium is often described as a “reflected†or “left-hand” version of Prilosec. They are both products of the pharmaceutical company AstraZeneca, and some parties have described Nexium as a “follow-up drug†to the wildly successful Prilosec; it was introduced just as Prilosec’s patent protection was about to expire.
The conditions they treat:
- Gastroesophageal reflux disease (GERD, commonly called acid reflux) is when the lining of the esophagus becomes inflamed from the regurgitation of stomach acid. Prilosec and Nexium can both treat GERD.
- Duodenal ulcers: Prilosec and Nexium can both treat duodenal ulcers that are caused by a Helicobacter pylori infection, but only Prilosec can treat duodenal ulcers caused by other factors.
- Gastric ulcers: Both drugs treat benign gastric ulcers, but Nexium is limited to treating such ulcers caused by nonsteroidal anti-inflammatory drugs. Prilosec can treat any type of gastric ulcer.
Your choices:
Prilosec is an older, more established drug, and thus has been approved to treat more conditions than Nexium has. If your condition is one that only Prilosec can treat, then your choice is crystal-clear.
However, if you are one of the millions of people whose condition is approved to be treated with either Prilosec or Nexium, then you have some research, discussion, and possibly even a trial run with the medication ahead of you. Someone suffering from acid reflux, for instance, would have a valid case to try either medication. If this is the case, discuss your particulars with your doctor for advice on which to start with.
The two drugs are so similar that many patients report choosing solely based on logistical factors such as availability and affordability. However, here are some other issues to consider in your comparison:
- Check your insurance plan: some cover both Prilosec and Nexium, while some only cover one choice.
- Prilosec has a generic version, while Nexium does not, which may affect your buying decision.
- Some people tolerate one drug better than its sibling; you may need to compare to learn what works for you.
- Prilosec can have a side effect of appetite loss, while this has not been reported with Nexium.
- Prilosec is generally recommended for shorter courses of treatment, while Nexium is often recommended for longer courses of 4-8 weeks.
These medications are very similar, but are not the same. Do not substitute. As with any drug, please consult your physician before taking.

Long-term sufferers of insomnia who have not found lasting relief from such sleep aids as Ambien or Sonta should consider researching Rozerem, the only medication of its type approved in the treatment of sleeplessness.
Rozerem (ramelteon) is the first of a new class of insomnia drugs: melatonin receptor agonists. These are similar to the naturally-produced sleep hormone melatonin, which your body needs for healthy sleep cycles. Rozerem, manufactured by Takeda Industries North America, was approved by the FDA in July 2005 for the treatment of delayed-onset insomnia. It emerged against a backdrop of other classes of drugs to treat the condition — and it has some important differences.
Insomnia was historically treated with barbiturates, which were extremely strong and frighteningly addictive. In the Sixties, the benzodiazepines appeared. These drugs (such as Halcion) helped treat insomnia with a much lower rate of serious side effects and addiction, but still had moderate side effects such as dizziness and a hangover effect. In the Nineties, there emerged a new class of non-benzodiazepine sleep aids, including Sonata and Lunesta, which have safely helped many people combat insomnia. Still, as they target several broad areas of the brain that are involved in sleep, they still have considerable side effects on memory and clarity.
In 2005, Rozerem was approved as a treatment for insomnia. It is said to have a different, more precise mechanism than other sleep aids, with an ability to target the “master clock†of the human body, affecting the sleep-wake cycle without unduly interfering with nearby brain functions.
Because it is in a different class than Lunesta and Ambien, Rozerem may be an effective treatment for patients who have not found lasting results on these medications. If you have not reconsidered your insomnia treatment since this important new class of drugs appeared in 2005, it is worth researching these new developments, as they may cure your insomnia more effectively, or do so with fewer side effects.
Side effects: Common side effects on this medication are dizziness, drowsiness, and daytime sleepiness. Sometimes people using this drug sleep-walk or perform other actions in their sleep. More serious side effects involve hormonal changes such as missed periods, nipple discharge, or difficulty becoming pregnant. It is important to tell your doctor immediately if you experience depressed or suicidal thoughts while taking this medication. Finally, be aware of any symptoms of a very serious allergic reaction to Rozerem such as a rash or swelling. Call your doctor immediately if this occurs.
Cautions and contra-indications: Rozerem is not suitable for patients with liver disease. You should not take it if you are also taking fluvoxamine, rifampin, or certain antifungal antibiotics. You should advise your doctor if you suffer from any breathing disorders such as sleep apnea or chronic obstructive pulmonary disease. You should also tell your doctor if you have a history of mental illness, depression, or suicidal thinking. And of these factors might mean that you cannot take Rozerem, or that you might have an adjusted dose. Rozerem is a pregnancy category C drug, so it may be harmful to an unborn baby, or in breast milk. Finally, Rozerem may affect hormonal levels in men and women, with possible effects to the desire and fertility. Talk with your doctor about your reproductive plans if you are considering Rozerem.
As with any drug, please consult your doctor before taking.
A diagnosis of high cholesterol can be intimidating, but there is a lot you can do to control this condition. In addition to modifying your diet and upping your exercise, the addition of a HMG-CoA Reductase Inhibitor — a class of drugs commonly called “statins†— can safely and effectively lower your cholesterol. (HMG-CoA Reductase helps our liver produce cholesterol; when the chemical is inhibited, the amount of cholesterol is correspondingly reduced.) For people with heart disease, statins can lower the risk of a cardiac event and subsequent death. If you and your doctor have determined that you need a statin, how can you pick the right statin for your needs?
There are six statins on the market: atorvastatin, fluvastatin, lovastatin, pravastatin, rosuvastatin, and simvastatin. They differ in their ability to reduce cholesterol, and they also differ in their rates of reducing heart attacks. Their costs are also quite different — and since most people take statins for a long time, the costs add up over the years. With all of these variables, choosing the right statin for you can be complex.
All statins are capable of lowering LDL (“badâ€) cholesterol and triglycerides, and raising HDL (“goodâ€) cholesterol. The statins do differ in how effectively they can do this, and it is highly dose-dependent. Says Drug Digest:
If the needed LDL-C reduction is up to 35-36%, any of the statins should be acceptable choices for therapy. For a desired reduction of LDL-C greater than 42%, simvastatin (Zocor), atorvastatin (Lipitor), or rosuvastatin (Crestor) would be needed.
Indeed, the best-known statins are Crestor, Lipitor, and Zocor (quite probably because they have the greatest effect on cholesterol levels). The latter two are also endorsed by Consumer Reports. Taking evidence for effectiveness, safety, and cost into account, the publication rated both of these statins as “Consumer Reports Best Buy Drugs.†They recommend:
• Generic simvastatin (20mg or 40 mg) — if you need 30% or greater LDL reduction and/or have heart disease or diabetes, or if you have had a heart attack or have acute coronary syndrome and your LDL level is not highly elevated.
• Atorvastatin (Lipitor) (40mg or 80mg) — if you have had a heart attack or have acute coronary syndrome and your LDL is highly elevated; use for two years and then reconfirm need or switch to generic simvastatin.
Charts on Drug Digest have some great comparisons. For instance, they show that Lipitor (10-80 mg.) can reduce total cholesterol by 25-45%, while Zocor (5-80 mg.) can reduce the same numbers by 19-36%, and Crestor (5-40 mg.) can reduce it by 33-46%. As for lowering HDL, Lipitor can offer reduction of 5-9%, Zocor lessens HDL by 8-16%, and Crestor lowers these numbers by 8-14%. As you can see, choosing the proper statin has a lot to do with which numbers (Total Cholesterol, HDL, LDL, or triglycerides) you are trying to effect.
A final consideration is that last year there was reporting on an observational study done by Pfizer that suggested that there were certain benefits to using Lipitor over Crestor. However, one must keep in mind that Pfizer conducted the study, and they are the manufacturer of Lipitor, and they are defending this drug against Merck’s Zocor product, which is now available in a generic formula. Here is the information as presented by The Wall Street Journal:
An analysis, published in the latest Clinical Therapeutics Journal, mined a large database of health-care records and found that patients taking Lipitor had a 12% lower risk of a cardiovascular event than those on simvastatin, the generic name for Zocor. The patients on Lipitor had a 15% lower risk of having a heart attack.
So-called observational studies like this one that look at data after the fact aren’t as powerful as prospective clinical trials. Jack Tu, a cardiologist who specializes in outcomes research at Canada’s Institute for Clinical Evaluative Sciences, says the latest Pfizer study didn’t take into account factors that could predispose a patient to heart problems, such as smoking and cholesterol levels. “Just on this alone, you wouldn’t recommend that everyone should switch onto Lipitor,†he says.
Still, Pfizer hopes that doctors will take notice. “We’ve done two rather large observational studies and patients have a lower risk of cardiovascular events on Lipitor [compared with] simvastatin,†says Susan Shiff, Pfizer’s team leader for cardiovascular outcomes. “Doctors need to factor this into discussions with patients.â€
You should definitely discuss with your physician which statin is right for you. In general, the best plan is to take the LOWEST dose of a statin that gets you to your target level for cholesterol. Overly large doses can be harmful to your liver and to your muscles. If you experience muscle aches and pains when taking a statin, contact your doctor immediately.
 Major depressive disorder affects approximately 15 million American adults in the U.S. in a given year, and a first pharmacological line of defense is often a prescription for an SSRI such as Prozac, Celexa, or Zoloft. (These drugs have been favored since the late 1980s for the treatment of depression as they are generally well tolerated, have fewer side effects than their predecessors the MAOIs, and help a great many people.)
Major depressive disorder affects approximately 15 million American adults in the U.S. in a given year, and a first pharmacological line of defense is often a prescription for an SSRI such as Prozac, Celexa, or Zoloft. (These drugs have been favored since the late 1980s for the treatment of depression as they are generally well tolerated, have fewer side effects than their predecessors the MAOIs, and help a great many people.)
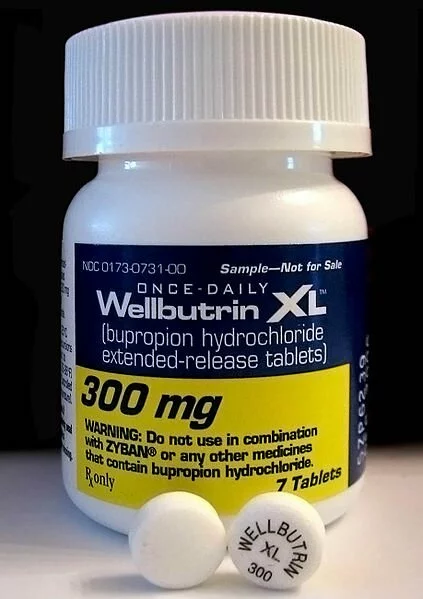
However, people suffering from atypical depression — characterized by hunger and sleepiness, rather than loss of appetite and insomnia — may have different needs in an antidepressant and should discuss with their doctor options such as Bupropion (familiarly known by its GlaxoSmithKline trade name, Wellbutrin), which could help where popular SSRIs might fail.
That is because SSRIs — Selective Serotonin Reuptake Inhibitors — work on the neurotransmitter Serotonin, while Wellbutrin — an NDRI — is a Norepinephrine and Dopamine Reuptake Inhibitor. This change of focus in the affected neurotransmitter may make all the difference for those individuals who suffer depression in an atypical manner.
Atypical depression differs from regular, “melancholic†depression primarily in energy and appetite. It is often characterized by “reversed vegetative symptoms†such as over-eating (regular depressives have little appetite) and/or over-sleeping (regular depression is usually characterized by sleeplessness).It is estimated that up to 40% of people suffering from depression have atypical symptoms.
Wellbutrin reportedly has a more enlivening affect than the SSRIs, so it is often considered for those who are sleeping abnormally long amounts. (For this reason, it is not advised for those suffering anxiety or agitation.) It is also one of the only antidepressants that is not associated with weight gain, and for this reason is also suitable for atypical depressives who may be overeating.
Even successful users of SSRIs have reason to consider Wellbutrin. SSRIs have widely-known sexual side effects that trouble some patients, even if the SSRI is curing their depression. This may make them turn to their physician for refinement of the prescription. Says Ray Sahelian, M.D.:
Since bupropion raises dopamine levels, it actually can enhance sexuality rather than depress libido as do many SSRIs. Bupropion has been shown to have a favorable effect on sexual dysfunction. Several reports and small, short-term trials have examined bupropion as an adjunct or substitute for other antidepressants in sexually dysfunctional patients. This means that Wellbutrin is often prescribed for sufferers of atypical depression, but it is also prescribed as an add-on for people using SSRIs who would like to try to combat the sexual side effects of SSRIs.
In other words, Wellbutrin is often prescribed as an add-on to an SSRI for the express purpose of relieving some of the SSRI’s sexual side effects (usually loss of libido or functioning).
Depression is not the only condition that Bupropion has been approved to treat. In 1997, it was approved by the FDA as a smoking cessation aid under the name Zyban. And in 2006, Wellbutrin XL was approved as a treatment for Seasonal Affective Disorder. Because both Wellbutrin (prescribed for depression) and Zyban (prescribed for smoking cessation) are essentially Bupropion, patients should not take both at the same time; they would be doubling their dose.
Caution: The most well-known side effect of Bupropion is that it lowers seizure thresholds. Doctors have worked around this with lower dosages (it is highly dose-dependent) and controlled-release formulations. Still, those with seizure disorders should avoid Bupropion. Other common side effects are nervousness/ agitation and insomnia. As with any antidepressant, people suffering from increased depressive symptoms or thoughts of suicide should contact their doctor immediately.
Some formulations of Bupropion are available as generics in the United States and Canada.
U.S. Brand Names
- Budeprion SR®
- Budeprion XL®
- Buprobanâ„¢
- Wellbutrin SR®
- Wellbutrin XL®
- Wellbutrin®
- Zyban®
Canadian Brand Names
- Novo-Bupropion SR
- PMS-Bupropion SR
- RATIO-Bupropion SR
- SANDOZ-Bupropion SR
- Wellbutrin XL®
- Wellbutrin®
- Zyban®
-
Search Blog Posts
-
Watch our YouTube Video
-
-
Trending Content
-

-
Categories
Big Pharma Buy prescriptions online Canadian drugs Drug costs Drug reimportation Drug safety eDrugSearch.com FDA Health 2.0 Healthcare100 Healthcare blogs Healthcare solutions Low-cost drugs Medicare Part D Merck Online pharmacies Online pharmacy safety Pfizer Pharma bloggers Pharmaceutical companies Pharmaceutical marketing Pharma cheerleaders Prescription drug abuse Prescription drug prices Prescription drugs Prescriptions Wal-Mart drug plan -
Blogroll
- Bullet Wisdom
- Bulverde Business Directory
- Christian Counseling San Antonio Tx.
- Christian Schools in San Antonio Texas
- Christian Social Network
- Christians United for Israel
- DrugWonks.com
- Eye on FDA
- GoozNews
- Health 2.0
- Hunting Forum
- In the Pipeline
- Jesus Christ Our King
- John Hagee Ministries
- Kevin, M.D.
- Local Search Marketing
- My $299 Website
- Pharm Aid
- Pharma Marketing
- PharmaGossip
- Pharmalot
- San Antonio Asphalt
- San Antonio Life Insurance
- San Antonio Pressure Washing
- Storage New Braunfels Tx
- Texas Wildlife Supply
- The Angry Pharmacist
- The Health Care Blog
- The Peter Rost Blog
- World Vision
-
Tags
big pharma Canadian drugs canadian pharmacies canadian pharmacy consumer reports craig newmark divine healing Drug costs drug prices Drug reimportation eDrugSearch.com FDA Fosamax Generic drugs healing scriptures Health 2.0 healthcare reform Hypertension Jehova Rophe Jesus Christ Lipitor Metformin miracles nabp online pharmacy dictionary online prescriptions osteoporosis peter rost Pharmacies pharmacists pharmacychecker pharmacy spam phrma Prescription drugs prescription medication Proverbs 3:5-8 reimportation relenza Roche saving money SSRI swine flu Tamiflu The Great Physician The Lord our Healer -
Recent Tweets
- New blog posting, How to Get the Cheapest Prescription Medications - http://t.co/iRBgRlYnsQ [#]
- Canadian Pharmacy | Canadian Pharmacies | Online Pharmacy Reviews: http://t.co/s51v4jpoCO [#]
- JanDrugs Reviews and Ratings at http://t.co/UnEmxPbzFa: http://t.co/zMR4qGA7o1 [#]
- eDrugSearch Blog Rank on the Healthcare100: http://t.co/VJprL4LZWl [#]
-
Archives
-
Recent Comments
- Heather Sturges on What is the Difference Between Effexor and Cymbalta?
- Lupe Machol on Cost of diabetes drugs has nearly doubled
- Manpower For Hospital In Pune on Why is Medicine Cheaper in Canada?
- Jen on How a Canadian Pharmacy Can Help You Offset Drug Price Hikes
- nino iarajuli on Vending machine dispenses prescription drugs